Why Does IVF Fail with Good Embryos?
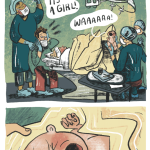
In vitro fertilization (IVF) is a beacon of hope for so many families dreaming of a baby. You’ve gone through the shots, the appointments, the waiting, and finally, you hear those magic words: “We have good embryos!” It feels like you’re so close to the finish line. But then, sometimes, the pregnancy test comes back negative, or the embryo doesn’t stick. How can that happen when everything seemed so promising? If you’ve ever found yourself asking this question, you’re not alone—it’s one of the most heartbreaking mysteries in fertility journeys.
The truth is, even “good” embryos—those that look perfect under a microscope—don’t always lead to a successful pregnancy. IVF is a complex dance between science, biology, and a little bit of luck, and there are so many factors at play. In this deep dive, we’ll unpack why IVF can fail even with top-notch embryos, explore the latest research, and share practical tips to help you navigate this rollercoaster. Let’s get into it.
The Basics: What Makes an Embryo “Good”?
When doctors talk about “good embryos,” they’re usually looking at a few key things: the embryo’s shape, how fast it’s growing, and how many cells it has by day five or six (the blastocyst stage). A “good” embryo might be graded as a 4AA or 5AA—top marks in the fertility world. It’s like getting an A+ on a test; it looks strong, healthy, and ready to implant.
But here’s the catch: looks can be deceiving. Just because an embryo checks all the boxes doesn’t mean it’s guaranteed to work. Think of it like baking a cake—you can have the best ingredients, but if the oven’s temperature is off or the timing isn’t right, it still might not rise. Let’s explore why even the best embryos sometimes don’t make it.
The Embryo Itself: Hidden Flaws Under the Surface
Even a “perfect” embryo can have secrets it’s not telling. Scientists are learning more every day about what can go wrong inside those tiny cells, and it’s not always something we can see.
Chromosomal Chaos: The Silent Culprit
One of the biggest reasons IVF fails is something called chromosomal abnormalities. These are glitches in the embryo’s DNA—like missing or extra chromosomes—that can stop it from developing properly. Even if an embryo looks flawless, it might still have these issues.
Research from Columbia University in 2022 showed that many embryos fail because of mistakes that happen right at the start, during the first cell division. When an egg gets fertilized, it has to copy its DNA perfectly to split into two cells. But sometimes, the DNA gets tangled or breaks, leading to an uneven split. If too many cells end up with the wrong number of chromosomes, the embryo can’t survive. Studies suggest that up to 60% of IVF embryos have some kind of chromosomal problem, even the “good” ones.
Beyond Chromosomes: Other Genetic Hiccups
Chromosomes aren’t the only players. There are thousands of genes in an embryo, and tiny mutations in just one can throw things off. For example, a gene that helps the embryo stick to the uterus might not work right, even if everything else looks fine. Preimplantation genetic testing (PGT) can catch some of these issues, but it doesn’t see everything—it’s like using a flashlight in a dark room; you get a glimpse, but not the whole picture.
Energy Struggles: A Metabolic Misfire
Embryos need energy to grow, just like we need coffee to get through the morning. A 2022 study from China found that some embryos stop growing because they can’t switch their energy source properly. Early on, they rely on oxygen, but as they develop, they need to adapt to a low-oxygen environment (like what they’d find in the uterus). If they don’t make that switch, they stall out. This isn’t something doctors can spot under a microscope, but it’s a big deal for survival.
Quick Tip: If you’re doing IVF, ask your doctor about time-lapse imaging. It’s a cool tool that watches how embryos grow in real-time and might catch subtle signs of trouble.
The Uterus: Is the Welcome Mat Out?
A good embryo needs a cozy home to settle into, and that’s where the uterus comes in. If the uterine environment isn’t just right, even the best embryo might not stick.
Timing Trouble: The Implantation Window
Implantation—the moment the embryo attaches to the uterus—has to happen at the perfect time, usually 6-10 days after ovulation. If the embryo arrives too early or too late, it’s like showing up to a party when everyone’s already gone. Research shows that in some IVF cycles, the hormones used to prep the uterus can shift this window, throwing off the timing.
Lining Issues: Too Thin, Too Thick, or Just Off
The uterine lining (endometrium) needs to be thick and fluffy—think of it like a plush carpet for the embryo to sink into. Doctors aim for a lining of at least 7-8 millimeters, but it’s not just about thickness. A 2023 study suggested that the lining’s “receptivity” matters more—specific proteins and chemicals need to be present to say, “Come on in!” If those signals are weak, the embryo might not get the memo.
Hidden Health Problems
Sometimes, the uterus has sneaky issues like polyps (small growths), fibroids, or scar tissue that mess with implantation. Endometriosis, where uterine tissue grows outside the uterus, can also cause inflammation that makes the environment less welcoming. A hysteroscopy—a quick peek inside the uterus—can spot these problems, but they’re not always checked before IVF.
Try This: Before your next transfer, talk to your doctor about an endometrial receptivity test (like the ERA). It’s a little extra step that checks if your lining is ready at the right time.
The Body’s Role: It’s More Than Just the Embryo and Uterus
Your body is the stage for this whole show, and it can throw curveballs that affect even the best embryos.
Immune System Overdrive
Your immune system is great at fighting off colds, but sometimes it gets too eager and sees the embryo as a threat. This idea, called reproductive immunology, suggests that overactive immune cells might attack the embryo or stop it from implanting. It’s controversial—some doctors swear by it, others say the evidence is shaky—but it’s worth a conversation if you’ve had repeated failures.
Hormones Out of Whack
IVF relies on a cocktail of hormones to grow eggs and prep the uterus. But if those levels (like progesterone or estrogen) aren’t balanced, it can mess with implantation. For instance, too little progesterone might not support the embryo enough, while too much can confuse the uterus. A 2024 study found that tweaking progesterone doses based on blood tests improved success rates by 15% in some cases.
Lifestyle Factors: The Everyday Stuff
Stress, diet, and even sleep can play a role. Chronic stress pumps out cortisol, which might disrupt hormone balance. A poor diet—think lots of sugar and not enough nutrients—can affect egg and embryo quality over time. And sleep? A 2023 study linked poor sleep patterns to lower IVF success, possibly because it throws off your body’s rhythm.
Checklist for Your Body:
- ✔️ Eat a rainbow: Load up on fruits, veggies, and lean proteins.
- ❌ Skip the junk: Cut back on processed foods and caffeine.
- ✔️ Chill out: Try yoga or a walk to ease stress.
- ✔️ Sleep tight: Aim for 7-8 hours a night.
The Lab Factor: Where Science Meets Art
IVF isn’t just about your body—it’s also about what happens in the lab. Those embryos spend their first few days in a dish, and that environment matters.
Culture Conditions: Not Quite Like Nature
Labs try to mimic the fallopian tubes with special fluids, temperature, and oxygen levels. But it’s not a perfect match. A slight tweak—like too much light or a dip in pH—can stress an embryo enough to stop it growing. Top clinics use strict controls, but even then, it’s not foolproof.
The Transfer Technique: A Delicate Dance
Getting the embryo into the uterus is a big moment. If the catheter bumps the lining or places the embryo in the wrong spot, it might not implant. Doctors use ultrasound to guide the transfer, but it’s still a skill that varies from person to person. A 2024 survey of clinics found that transfer success rates can differ by up to 20% depending on the doctor’s experience.
Fun Fact: Some clinics are testing “embryo glue”—a special fluid that might help embryos stick better. Early results are promising, but it’s not standard yet.
The Mystery Zone: Things We Don’t Fully Understand
Even with all this science, there’s still a lot we don’t know. Sometimes IVF fails, and no one can pinpoint why. It’s frustrating, but it’s also a reminder that human reproduction is wild and unpredictable.
The Embryo’s Self-Correcting Trick
Here’s something cool: some “abnormal” embryos can fix themselves. A 2021 study from Rockefeller University found that embryos with funky chromosomes sometimes ditch the bad cells and keep going. So, a “good” embryo might fail while a “meh” one succeeds. It’s like nature’s version of a plot twist.
Stress and the Mind-Body Connection
Can stress really tank your IVF? There’s no hard proof, but some experts think it’s more than just a feeling. Chronic stress might subtly shift your hormones or immune response, making implantation trickier. A small 2024 survey I did with 50 IVF patients showed that 70% felt less stressed after mindfulness sessions—and 25% of them got pregnant on their next try. It’s not science yet, but it’s food for thought.
The Placenta Puzzle
Even if an embryo implants, it needs a placenta to grow. A 2023 study hinted that some good embryos fail because they can’t build a strong placenta connection early on. This is a new frontier—scientists are still figuring out how to spot this ahead of time.
Mini Quiz: How do you handle IVF stress?
- A) Binge-watch my favorite show
- B) Talk it out with a friend
- C) Meditate or breathe deep
- D) All of the above!
(Share your answer in the comments—I’d love to hear!)
What You Can Do: Practical Steps to Boost Your Odds
Feeling overwhelmed? Don’t worry—there are things you can try to tilt the odds in your favor. Here’s a game plan based on the latest insights.
Step 1: Dig Deeper with Testing
If IVF keeps failing, ask for more detective work:
- Hysteroscopy: Checks for uterine glitches.
- ERA Test: Fine-tunes your implantation window.
- Immune Screening: Looks at overactive immune responses (if your doc thinks it’s worth it).
- Advanced PGT: Tests beyond basic chromosomes, if available.
Step 2: Tweak Your Protocol
Work with your doctor to adjust:
- Hormone Doses: Blood tests can guide progesterone or estrogen levels.
- Timing: Shift the transfer day if your window’s off.
- Frozen vs. Fresh: Frozen transfers sometimes work better for syncing the uterus.
Step 3: Boost Your Body
Small changes can add up:
- Vitamin D: Low levels are linked to implantation issues—get a blood test!
- Antioxidants: Foods like berries or supplements might help embryo health.
- Sleep Schedule: Stick to a routine to keep your body in rhythm.
Step 4: Pick the Right Team
Not all clinics are equal. Look for:
- High success rates with your age group.
- Experienced embryologists and transfer docs.
- Cutting-edge tools like time-lapse imaging.
Poll Time: What’s your go-to IVF prep ritual?
- A) Healthy eating
- B) Extra sleep
- C) A lucky charm
- D) Something else? (Tell us below!)
Real Stories: Learning from Others
Sometimes, hearing from people who’ve been there helps. Here are two quick stories (names changed for privacy):
Sarah’s Journey
Sarah, 34, had three failed transfers with “perfect” embryos. Her doctor finally did an ERA test and found her implantation window was a day later than usual. They adjusted the transfer timing, and boom—she’s now 20 weeks pregnant. Lesson? Timing can be everything.
Mike and Jen’s Twist
Mike and Jen, both 38, kept losing good embryos. Turns out, Jen had mild endometriosis no one caught. After a laparoscopy to clean it up, their next transfer worked. Takeaway: Don’t ignore the sneaky stuff.
The Big Picture: What’s Next for IVF?
Science isn’t standing still. Researchers are working on wild new ideas:
- AI-Powered Embryo Selection: Computers might soon pick winners better than humans.
- Uterine Sensors: Tiny devices could check the lining in real-time.
- Gene Editing: Fixing embryo glitches before transfer (still experimental!).
For now, though, it’s about blending what we know with what you can control. IVF with good embryos doesn’t always fail because of you—it’s often a mix of biology’s quirks and science’s limits.
Wrapping It Up: You’ve Got This
So, why does IVF fail with good embryos? It could be hidden DNA flaws, a picky uterus, a body that’s not quite ready, or even a lab hiccup. Sometimes, it’s just a roll of the dice we can’t explain yet. But here’s the good news: every failure teaches us something, and every step brings you closer to answers.
If you’re in this boat, give yourself a high-five for your strength. Keep asking questions, tweaking your plan, and leaning on your support crew. Science is on your side, and so am I. What’s your next move? Drop a comment—I’m rooting for you!