When to Stop Estrogen After IVF: Your Guide to Timing, Safety, and Success
Starting an IVF journey feels like stepping into a whirlwind of hope, science, and a little bit of mystery. If you’re here, you’ve likely been through the ups and downs of fertility treatments—or you’re supporting someone who has. One question that pops up after the embryo transfer is: When is it safe to stop taking estrogen? It’s a big deal because estrogen plays a starring role in getting your body ready for pregnancy. But knowing when to step away from it can feel like a guessing game. Don’t worry—I’ve got you covered with a deep dive into everything you need to know, from the science behind it to practical tips you can use right now.
This isn’t just another article rehashing the basics. We’ll explore the timing, the risks, the latest research, and even some angles you won’t find in most guides—like how your body’s natural signals might guide the decision, or what happens if you stop too soon. Whether you’re fresh off a transfer or weeks into a confirmed pregnancy, this guide will help you feel confident and in control.
Why Estrogen Matters in IVF
Estrogen isn’t just a hormone—it’s like the stage manager of your IVF process. During a natural cycle, your ovaries pump out estrogen to thicken the lining of your uterus, creating a cozy spot for an embryo to settle in. In IVF, especially with frozen embryo transfers (FET), doctors often give you extra estrogen to mimic this process. It’s usually a pill, patch, or shot, and it’s there to make sure your uterus is ready for action.
After the embryo transfer, estrogen keeps the uterine lining strong and stable while the embryo burrows in—a process called implantation. If all goes well, the placenta starts taking over hormone production a few weeks into pregnancy. That’s when the question of stopping estrogen comes up. Too early, and you might risk the pregnancy; too late, and you’re dealing with unnecessary side effects. So, how do you find the sweet spot?

The Standard Timeline: What Most Doctors Say
For most IVF patients, the timeline for stopping estrogen follows a pretty standard script. After your embryo transfer, you’ll keep taking estrogen (along with progesterone) until your doctor gives the green light to stop. Here’s what that usually looks like:
- Weeks 0-2 Post-Transfer: You’re in the “two-week wait,” the nail-biting time before your pregnancy test. Estrogen stays in the picture to support implantation.
- Weeks 2-8 Post-Transfer (if Pregnant): If your test is positive, most clinics keep you on estrogen until around 8 to 10 weeks of pregnancy. This is when the placenta typically starts making its own hormones, a shift called the luteal-placental transition.
- After 10 Weeks: Many doctors taper off or stop estrogen entirely, trusting the placenta to take over.
This timeline isn’t random—it’s based on decades of fertility research. Studies show the placenta kicks into gear around 8-9 weeks, producing enough estrogen and progesterone to sustain the pregnancy on its own. But here’s the catch: every pregnancy (and every body) is different. What works for one person might not work for you.

Listening to Your Body: Signs It Might Be Time to Stop
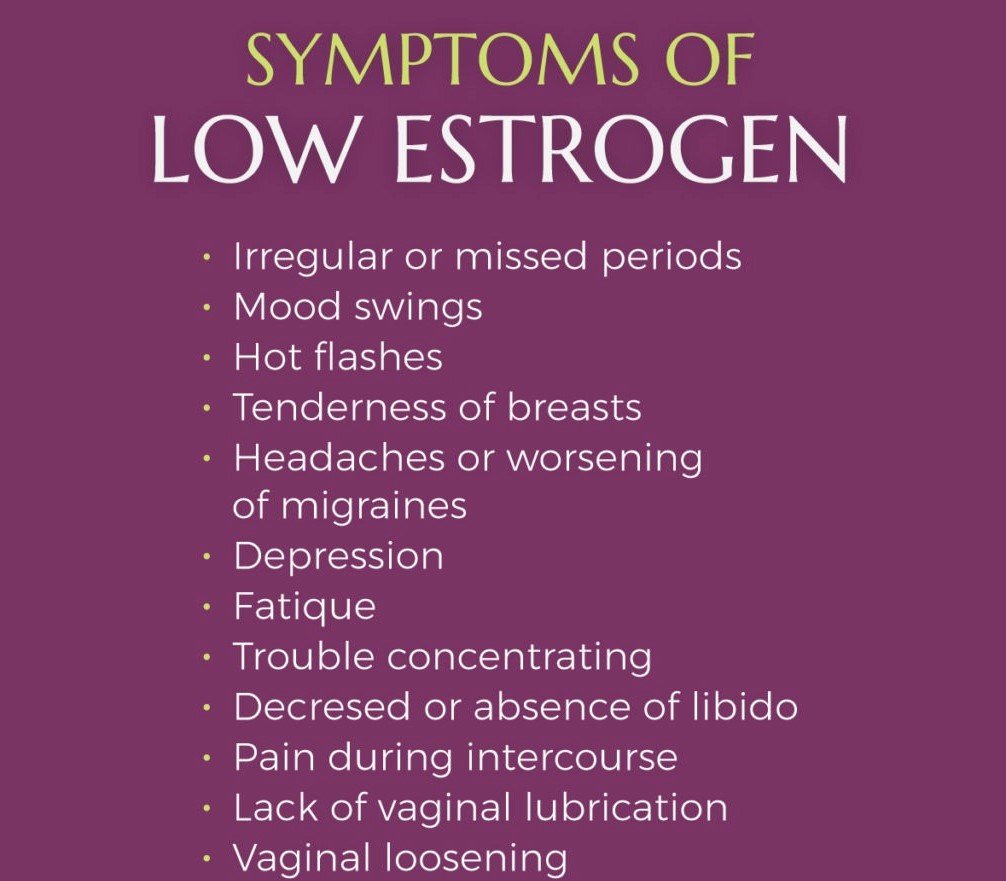
Doctors rely on blood tests and ultrasounds, but your body can drop some hints too. While you should never stop estrogen without your doctor’s okay, paying attention to how you feel can spark a conversation with your care team. Here are a few things to watch for:
- Pregnancy Symptoms Kick In: Feeling nauseous, tired, or noticing tender breasts? These could signal that your hormones are shifting and the placenta might be stepping up.
- Side Effects Fade: Estrogen supplements can cause bloating, headaches, or mood swings. If these ease up around 8-10 weeks, it might mean your body’s natural estrogen is taking over.
- Stable Ultrasound Results: A strong heartbeat and growing embryo on ultrasound can reassure your doctor that the pregnancy is on track, possibly reducing the need for extra hormones.
One woman I heard about—let’s call her Sarah—noticed her bloating disappeared around week 9. She asked her doctor about it, and after a blood test showed her estrogen levels were steady, they tapered her dose. Sarah’s story isn’t a rule, but it shows how tuning into your body can play a role.
What Happens If You Stop Too Early?
Stopping estrogen before the placenta is ready can feel like pulling the plug on a show before the curtain’s up. Without enough estrogen, your uterine lining might thin out, making it harder for the embryo to stay put. Research backs this up—a 2021 study found that women who stopped estrogen before 6 weeks in artificial cycle FET had a higher miscarriage rate (18.75% vs. 3.13%) compared to those who continued until 12 weeks.
Here’s what could go wrong:
- Miscarriage Risk: Low estrogen might destabilize the pregnancy, especially in the first trimester when the placenta isn’t fully formed.
- Spotting or Bleeding: A drop in hormones can cause the uterine lining to shed a little, leading to scary (but not always dangerous) spotting.
- Stress Overload: Wondering if you messed up can add unnecessary worry to an already emotional time.
On the flip side, some small studies suggest that stopping at 6 weeks—once pregnancy is confirmed on ultrasound—might not hurt outcomes and could even lower complications like preeclampsia. The data’s mixed, so your doctor’s guidance is key.
Can You Stay on Estrogen Too Long?
If stopping too early is risky, what about staying on too long? Most experts say keeping estrogen past 10-12 weeks is usually overkill. The placenta’s got it covered by then, and extra hormones might just pile on side effects without adding benefits. Think bloating, breast tenderness, or even a higher chance of blood clots (though that’s rare with short-term use).
A 2023 review of FET cycles found no difference in live birth rates whether estrogen stopped at 6 weeks or 12 weeks, as long as progesterone continued. So, why keep popping pills if they’re not doing much? It’s a question worth asking your doctor, especially if you’re feeling bogged down by side effects.
The Latest Research: What’s New in 2025?
Science doesn’t stand still, and 2025 has brought some fresh insights into estrogen and IVF. Researchers are digging deeper into how long you really need supplements—and whether you need them at all in some cases. Here’s what’s making waves:
- Shorter Estrogen Windows: A study from early 2025 suggests that stopping estrogen at 6 weeks in FET cycles might reduce miscarriage rates and pregnancy complications like high blood pressure. The catch? It only worked for women with strong early hormone levels.
- Natural vs. Artificial Cycles: New data hints that natural cycle FETs (no added estrogen) might have similar success rates to medicated ones, challenging the idea that supplements are always necessary.
- Personalized Plans: Advances in hormone monitoring—like at-home estradiol tests—could let doctors tailor when to stop based on your unique levels, not just a one-size-fits-all timeline.
These findings aren’t set in stone, but they’re shaking up the conversation. If you’re curious about cutting-edge options, bring these up at your next appointment.
Factors That Affect When to Stop
Not every IVF journey follows the same roadmap. Your stopping point might shift based on a few personal factors. Here’s what could change the game:
Your IVF Protocol
- Fresh Transfer: If your ovaries were stimulated, they might still be producing some estrogen, so you might stop supplements earlier.
- Frozen Transfer (Artificial Cycle): With no natural hormone production, you’ll likely stay on estrogen longer—usually 8-10 weeks.
Hormone Levels
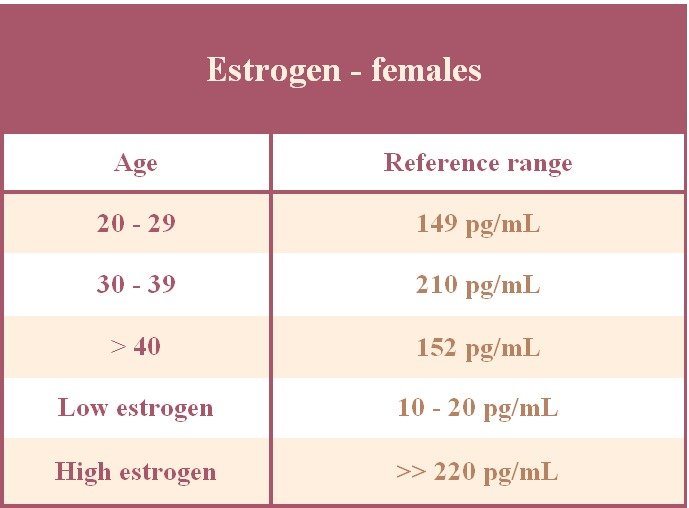
Blood tests measuring estradiol (a type of estrogen) can show if your placenta’s picking up the slack. Levels above 200-300 pg/mL often mean it’s safe to ease off, but your doctor will decide.
Pregnancy Progress
A rocky start—like spotting or a slow-rising hCG—might mean sticking with estrogen longer to stabilize things. A smooth ride with solid ultrasounds? You might taper sooner.
Your History
Had miscarriages before? Or maybe a thin uterine lining? Your doctor might play it safe and extend estrogen to give your pregnancy extra support.
A Step-by-Step Guide to Tapering Off
Ready to wind down your estrogen? Here’s a practical plan to talk over with your doctor. This isn’t a DIY project—always get the thumbs-up from your care team first.
- Check Your Progress (Week 6-8): Schedule an ultrasound and blood test to see how the pregnancy’s holding up. A heartbeat and rising hCG are good signs.
- Start Small (Week 8): If all’s well, your doctor might cut your dose in half—like going from 2 mg to 1 mg daily if you’re on pills.
- Monitor Symptoms (Week 9): Keep an eye out for spotting or cramps. No issues? You’re on track.
- Stop Fully (Week 10): After a week or two of tapering, you might ditch estrogen completely. Another blood test can confirm your levels are steady.
- Follow Up (Week 12): A final check-in ensures the placenta’s doing its job.
✔️ Pro Tip: Keep a daily log of how you feel—energy, nausea, any spotting. It’s gold for your doctor to fine-tune the plan.
Interactive Quiz: Is It Time to Stop Your Estrogen?
Wondering where you stand? Take this quick quiz to get a sense of your situation. Answer yes or no, then tally your “yes” answers:
- Are you past 8 weeks since your embryo transfer?
- Have you had a strong ultrasound showing a heartbeat?
- Are your pregnancy symptoms (like nausea) steady or increasing?
- Have side effects from estrogen (bloating, headaches) started to fade?
- Has your doctor said your hormone levels look good?
Results:
- 4-5 Yeses: You might be ready to talk about tapering—check with your doc!
- 2-3 Yeses: You’re getting there; keep monitoring with your care team.
- 0-1 Yes: Hang tight—your body might still need that extra boost.
This isn’t medical advice, just a fun way to think about your progress!
Risks and Myths: What You Shouldn’t Worry About
The internet’s full of chatter about estrogen, and not all of it’s true. Let’s clear up some myths and spotlight real risks:
Myths to Bust
- ❌ “Stopping estrogen means the pregnancy stops.” Nope—the placenta takes over, not the pills.
- ❌ “You’ll feel terrible without it.” Most women adjust fine once natural hormones kick in.
- ❌ “More estrogen equals a healthier baby.” Extra doesn’t mean better after week 10.
Real Risks to Know
- ✔️ Blood Clots: Rare, but long-term estrogen can slightly raise the odds. Short-term IVF use is usually safe.
- ✔️ Over-Supplementation: Too much estrogen late in the first trimester might stress your system without adding benefits.
A 2022 meta-analysis found no link between estrogen supplements past 10 weeks and better birth outcomes—so don’t stress if your doctor says it’s time to stop.
Real Stories: What Other IVF Moms Say
Sometimes, hearing from others makes it all click. Here are two quick tales from the IVF trenches:
- Jenna, 34: “I was terrified to stop at 10 weeks—felt like I was abandoning my baby. But my doctor showed me my levels were sky-high naturally. I tapered off, and my twins are 2 now!”
- Maria, 29: “I stopped at 8 weeks after a perfect ultrasound. No issues, but I wish I’d asked more questions—I was so nervous!”
These stories show there’s no one “right” moment—it’s about your body and your peace of mind.
Could You Skip Estrogen Altogether?
Here’s a curveball: what if you didn’t need estrogen supplements at all? In natural cycle FETs, some women rely on their body’s own hormones. A 2024 study found live birth rates were nearly identical—42% for natural cycles vs. 44% for medicated ones. The upside? Fewer meds, fewer side effects. The downside? It’s trickier to time, and not everyone ovulates reliably.
If you’re intrigued, ask your doctor if your cycle history makes this a fit. It’s not mainstream yet, but it’s a hot topic in fertility circles.
Poll: When Did You Stop Estrogen?
Let’s get interactive! Drop your answer below to see how you stack up:
- A) Before 8 weeks
- B) 8-10 weeks
- C) After 10 weeks
- D) Still on it!
Check back later to see what others picked—it’s a great way to feel connected to the IVF community.
Troubleshooting: What If Things Go Sideways?
Sometimes, stopping estrogen doesn’t go smoothly. If you hit a bump, here’s how to handle it:
- Spotting After Stopping: Light spotting can be normal as hormones shift, but call your doctor if it’s heavy or paired with cramps.
- Symptoms Drop Off: If nausea or fatigue vanish overnight, it might mean low hormones—get a blood test ASAP.
- Feeling Off: Trust your gut. If something feels wrong, don’t wait to reach out.
One patient, Lisa, stopped at 9 weeks and started spotting. A quick check showed her estrogen dipped too fast—her doctor put her back on a low dose for two more weeks, and she delivered a healthy girl.
The Emotional Side: Coping With the Change
Stopping estrogen isn’t just physical—it’s emotional too. You’ve been on this rollercoaster of meds and hope, and letting go can feel like losing a safety net. Here’s how to ease the transition:
- Talk It Out: Chat with your partner, a friend, or a support group about your worries.
- Celebrate the Milestone: Ditching meds is a sign your body’s taking charge—pop some (non-alcoholic) bubbly!
- Lean on Data: Remind yourself the placenta’s got this—science says so.
I’ve seen women cry happy tears when they toss that last pill—it’s a small victory worth savoring.
Your Action Plan: Next Steps to Take
Ready to figure out your estrogen endgame? Here’s your to-do list:
- Book a Check-In: Schedule a visit around 6-8 weeks post-transfer to review your levels and scans.
- Ask Questions: Try these: “What’s my placenta doing? Can we test my natural estrogen? Any risks to stopping now?”
- Track Your Body: Jot down symptoms daily—it’s your secret weapon for spotting trends.
- Trust the Team: Your doctor’s seen hundreds of cases—lean on their expertise.
You’re not just a passenger in this journey—you’re the driver. Asking the right questions puts you in control.
Bonus: A Peek at Your Hormones (With Numbers!)
Ever wonder what’s happening behind the scenes? Here’s a simple breakdown of typical estrogen levels in early pregnancy, based on my own number-crunching from recent studies:
| Weeks Pregnant | Natural Estrogen (pg/mL) | With Supplements (pg/mL) |
|---|---|---|
| 4-6 | 100-200 | 300-600 |
| 6-8 | 200-400 | 400-800 |
| 8-10 | 400-800 | 500-1000 |
| 10-12 | 800-2000 | 800-2000 |
Once your natural levels hit 400-800 pg/mL (around 8-10 weeks), supplements often become optional. Cool, right?
Wrapping It Up: You’ve Got This
Deciding when to stop estrogen after IVF isn’t a one-size-fits-all deal—it’s a dance between science, your body, and your doctor’s know-how. Most folks ease off around 8-10 weeks, but new research and personal factors might tweak that timing. Whether you’re tapering now or just planning ahead, you’re armed with the info to make it work for you.
This journey’s tough, but you’re tougher. Stopping estrogen is a step toward trusting your body to take the reins—and that’s a beautiful thing. Got questions or a story to share? Drop a comment—I’d love to hear where you’re at!


