When Did IVF Begin? A Deep Dive into the History, Science, and Impact of In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might’ve heard tossed around in conversations about starting a family or in news stories about medical breakthroughs. It’s a process that’s helped millions of people become parents when nature alone wasn’t enough. But have you ever wondered where it all started? When did this incredible journey of creating life in a lab begin, and how has it shaped the world we live in today? Buckle up, because we’re about to take a fascinating trip back in time—way before test tubes and petri dishes became household names—to uncover the roots of IVF and explore how it’s evolved into the life-changing technology it is now.
The Birth of an Idea: Early Steps Toward IVF
IVF didn’t just pop up overnight. Its story begins long before the first “test-tube baby” made headlines. Picture this: it’s the late 1800s, and scientists are just starting to figure out how life begins at the tiniest level. One of the earliest pioneers was a guy named Walter Heape, a British scientist with a knack for experimenting with rabbits. In 1890, he pulled off something pretty wild—he took an embryo from one rabbit and transferred it to another, resulting in a successful pregnancy. This wasn’t IVF as we know it (no petri dishes here!), but it was a huge hint that embryos could be moved around and still grow into healthy babies.
Fast forward to the 1930s, and another scientist, Gregory Pincus, enters the scene. You might know him as one of the brains behind the birth control pill, but he was also obsessed with fertilizing eggs outside the body. In 1934, Pincus and his colleague Ernst Enzmann tried fertilizing rabbit eggs in a lab. They claimed success, but here’s the catch: later research showed the eggs might’ve been fertilized inside the rabbit before they were removed. Still, their work got people thinking—could this actually work for humans?
Then, in 1959, a breakthrough happened. Min Chueh Chang, working at the Worcester Foundation in Massachusetts, proved that rabbit eggs fertilized in a lab could grow into healthy baby rabbits when transferred back into a mother. Chang’s experiment was a game-changer—it showed that “in vitro” (Latin for “in glass”) fertilization wasn’t just a sci-fi dream. These early steps laid the groundwork for what would come next, but it’d take a few more decades—and some brilliant minds—to make IVF a reality for humans.
The Big Moment: 1978 and the First IVF Baby
July 25, 1978, is the date everyone remembers. That’s when Louise Joy Brown, the world’s first IVF baby, was born in Oldham, England. Her arrival wasn’t just a birth—it was a revolution. Louise’s parents, Lesley and John Brown, had been trying to have a baby for nine years, but blocked fallopian tubes made it impossible the natural way. Enter two trailblazers: Dr. Patrick Steptoe, a gynecologist, and Dr. Robert Edwards, a physiologist. These guys teamed up in the late 1960s with a bold idea—fertilize an egg outside the body and put it back in the womb.
Their process was nothing short of daring. Steptoe used a technique called laparoscopy (a fancy way of saying he peeked inside Lesley’s abdomen with a tiny camera) to retrieve her eggs. Edwards then mixed those eggs with John’s sperm in a lab dish. After a few days, they transferred the tiny embryo back into Lesley’s uterus. Nine months later, Louise arrived via C-section, weighing a healthy 5 pounds, 12 ounces. The world went nuts—some called it a miracle, others worried it was “playing God.” Edwards even won a Nobel Prize in 2010 for his work (sadly, Steptoe had passed away by then and couldn’t share the honor).
But here’s something cool that doesn’t always get mentioned: Louise wasn’t the only “first.” Just 67 days later, on October 3, 1978, a baby named Durga was born in India through IVF, thanks to Dr. Subhash Mukhopadhyay. He worked with basic tools—even a household fridge!—and didn’t get the recognition he deserved until years later. These twin milestones in 1978 mark the true beginning of IVF as a practical solution for infertility.
How IVF Works: A Peek Under the Hood
So, what exactly goes into making an IVF baby? It’s not as simple as mixing stuff in a dish and crossing your fingers. The process has evolved a ton since 1978, but the basics are still the same. Here’s a quick rundown:
- Step 1: Boosting Egg Production
A woman gets hormone shots to make her ovaries produce multiple eggs instead of the usual one per month. More eggs mean more chances for success. - Step 2: Egg Retrieval
Doctors use a thin needle guided by ultrasound to gently pull the eggs out of the ovaries. It’s quick, but it can be a little uncomfortable. - Step 3: Fertilization
In a lab, the eggs meet the sperm. Sometimes it’s a natural mingle in a dish; other times, a scientist injects a single sperm into an egg (that’s called ICSI—intracytoplasmic sperm injection). - Step 4: Embryo Growth
The fertilized eggs grow into embryos over a few days. Lab experts keep a close eye to pick the healthiest ones. - Step 5: Transfer Time
One or more embryos are placed into the uterus using a thin tube. If all goes well, one sticks around and grows into a baby.
Today, about 65-80% of eggs fertilize successfully, and success rates can hit nearly 50% for women under 35. That’s a far cry from the single-digit odds Steptoe and Edwards faced!
Beyond 1978: Milestones That Shaped IVF
IVF didn’t stop with Louise. The years after 1978 brought jaw-dropping advances that made it more effective and accessible. Here are some highlights:
- 1983: Donor Eggs Open New Doors
A woman with premature ovarian failure gave birth using a donated egg—the first time IVF helped someone whose ovaries couldn’t produce eggs. This was huge for older women or those with medical conditions. - 1990: Screening Embryos for Genetic Issues
Preimplantation genetic diagnosis (PGD) debuted, letting doctors check embryos for conditions like cystic fibrosis before transfer. It’s like a sneak peek to ensure a healthier baby. - 1992: ICSI Saves the Day for Male Infertility
A single sperm injected directly into an egg? That’s ICSI, and it’s been a lifeline for men with low sperm counts or motility issues. - 2000s: Freezing Becomes Routine
Freezing eggs, sperm, and embryos got way better, letting people delay parenthood or save extras for later tries. Today, frozen embryo transfers often work as well as fresh ones.
Each leap pushed IVF further, turning it from a long shot into a go-to option for all kinds of families—straight couples, single parents, same-sex partners, you name it.
Why Did IVF Take So Long to Happen?
You might be wondering—if scientists were messing with rabbit eggs in the 1930s, why’d it take until 1978 for a human IVF baby? Great question! A few roadblocks slowed things down:
- Tech Trouble
Early labs didn’t have the fancy tools we do now—like precise hormone controls or ultrasound. It was trial and error with clunky equipment. - Biology Mysteries
Figuring out how sperm and eggs actually work took time. For example, sperm need to “mature” (a process called capacitation) before they can fertilize an egg—something scientists nailed down in the 1950s. - Ethics and Pushback
People freaked out about “test-tube babies.” Religious groups, governments, and even some scientists worried it was unnatural. In the U.S., laws like the Dickey-Wicker Amendment still limit federal funding for embryo research, slowing progress.
Despite the hurdles, Steptoe, Edwards, and others kept at it, driven by the hope of helping families grow. Their grit paid off big time.
IVF Today: Numbers That Tell the Story
IVF has come a long way since 1978, and the stats prove it. By 2018, over 8 million babies had been born worldwide through IVF and other assisted reproductive technologies. In the U.S. alone, IVF accounts for 1-2% of all births each year—that’s over 76,000 babies in 2016! Success rates have soared too. For women under 35, nearly half of IVF cycles lead to a live birth, according to the CDC. Compare that to the 6% chance per cycle back in the early days.
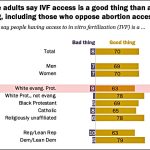
But it’s not all rosy. IVF can cost $12,000 to $25,000 per cycle, and insurance doesn’t always cover it. That’s why some folks are pushing for better access—think of the 2025 White House plan to make IVF more affordable. It’s a hot topic on platforms like X, where people share stories of hope, frustration, and everything in between.
Interactive Quiz: How Much Do You Know About IVF History?
Let’s test your knowledge with a quick quiz! Grab a pencil or just keep score in your head.
- In what year was the first human IVF baby born?
A) 1968
B) 1978
C) 1988 - Who was the first IVF baby?
A) Louise Brown
B) Durga Mukhopadhyay
C) Lesley Steptoe - What animal did Walter Heape use in his 1890 embryo transfer experiment?
A) Mice
B) Rabbits
C) Sheep
Answers: 1-B, 2-A (though Durga was a close second!), 3-B. How’d you do? Share your score with a friend and see who’s the IVF history champ!
The Unsung Heroes: Lesser-Known IVF Pioneers
Louise’s story gets all the spotlight, but plenty of other brilliant minds helped IVF take off. Take Miriam Menkin, for instance. In the 1940s, working with Dr. John Rock in Boston, she became the first person to fertilize a human egg in a lab. Her work was painstaking—think hours hunched over a microscope with no fancy tech to help. She didn’t get a baby out of it, but she proved it could be done.
Then there’s Subhash Mukhopadhyay in India. While Steptoe and Edwards were making headlines, he quietly delivered Durga in 1978. He faced skepticism and red tape, and tragically, he took his own life in 1981 before the world recognized his genius. These unsung heroes remind us that IVF’s story is global, messy, and full of human spirit.
IVF’s Ripple Effect: More Than Just Babies
IVF isn’t just about making families—it’s reshaped science, society, and even how we think about life. Here’s how:
- Medical Spin-Offs
Techniques like embryo freezing and genetic screening have spilled over into cancer care (preserving fertility before chemo) and stem cell research. IVF’s a gift that keeps on giving. - Family Diversity
Single moms, LGBTQ+ couples, and people using surrogates owe a lot to IVF. It’s broken the mold of what a “typical” family looks like. - Big Questions
IVF sparked debates about ethics—like what happens to unused embryos? Some see them as potential life; others don’t. It’s a convo that’s still going strong.
One wild stat: experts predict that by 2100, assisted reproductive tech (including IVF) could account for 400 million people alive—3% of the world’s population! That’s the kind of impact we’re talking about.
What’s Next for IVF? Peeking Into the Future
IVF’s past is amazing, but its future might blow your mind. Scientists are tinkering with ideas that sound straight out of a movie:
- Artificial Wombs
Imagine growing a baby outside the body entirely. It’s not here yet, but animal studies (like lamb fetuses in “biobags”) hint it’s possible down the road. - Gene Editing
Tools like CRISPR could let us tweak embryos to prevent diseases—or even pick traits. It’s controversial, but the tech’s advancing fast. - IVF for All Ages
New research on egg quality (think Coenzyme Q10 boosting older eggs) might help women in their 40s or 50s have biological kids more easily.
A 2022 study in Cureus highlighted how drugs like letrozole are cutting IVF costs and boosting egg yields, especially for breast cancer patients preserving fertility. It’s practical stuff that’s already changing lives.
Poll Time: What’s Your Take on IVF’s Future?
What do you think IVF should focus on next? Vote below and chat about it with your crew!
- A) Cheaper treatments
- B) Better success rates
- C) Ethical guidelines
- D) Crazy new tech (like artificial wombs)
No wrong answers—your voice matters!
Real Stories: IVF Up Close and Personal
Numbers and science are cool, but the heart of IVF is in the people it touches. Meet Sarah, a 38-year-old teacher from Ohio. After three years of trying naturally, she and her husband turned to IVF in 2022. “The shots were tough, and the waiting was torture,” she says. “But when I saw my son’s heartbeat on that screen, every penny and tear was worth it.” Their little guy, Ethan, just turned one.
Then there’s Javier, a single dad in California. He used IVF with a donor egg and surrogate in 2023. “I never thought I’d be a parent,” he admits. “IVF gave me my daughter, Luna. She’s my whole world.” These stories show IVF’s power—it’s not just a procedure; it’s a lifeline.
Busting Myths: What IVF Isn’t
IVF gets a lot of buzz, but some ideas floating around are flat-out wrong. Let’s clear the air:
- Myth #1: IVF Babies Are ‘Unnatural’
Nope! They’re conceived differently, but once they’re growing, it’s the same biology as any pregnancy. Studies show IVF kids are just as healthy as their peers. - Myth #2: It’s Only for Rich People
It’s pricey, sure, but costs are dropping, and some states (like New York) mandate insurance coverage. Plus, clinics offer payment plans. - Myth #3: It Always Works
Sadly, no. Even with top-notch care, success isn’t guaranteed—especially as you age. For women over 40, rates dip below 15% per cycle.
Knowing the truth helps you see IVF for what it really is: a tool with limits, but also incredible potential.
IVF Around the World: A Global Snapshot
IVF’s journey isn’t the same everywhere. In Japan, it’s super common—over 5% of babies born in 2015 came from IVF, thanks to high infertility rates and great tech. In Costa Rica, it was banned until 2015 because of embryo protection laws, showing how culture shapes access. Meanwhile, Australia lifted restrictions on single women and lesbians using IVF in 2002, paving the way for more inclusive policies.
Here’s a quick table to compare:
| Country | IVF Babies (% of Births) | Fun Fact |
|---|---|---|
| U.S. | 1-2% | Over 1 million IVF babies by 2015 |
| Japan | 5%+ | World leader in IVF cycles |
| Australia | ~3% | Early adopter of inclusive laws |
Wherever you are, IVF’s story reflects local vibes—science meets society in fascinating ways.
Tips for Anyone Considering IVF
Thinking about IVF? It’s a big step, but you don’t have to go in blind. Here’s some down-to-earth advice:
✔️ Do Your Homework
Research clinics—look at success rates, reviews, and costs. The CDC has a handy tool for comparing U.S. clinics.
✔️ Talk It Out
Chat with your partner, friends, or a counselor. IVF’s emotional rollercoaster is easier with support.
✔️ Boost Your Odds
Eat well, cut stress, and skip smoking. A 2023 study found lifestyle tweaks can up your chances by 10-15%.
❌ Don’t Rush
Take time to weigh options—IVF’s not the only path. Adoption or other treatments might fit too.
❌ Don’t Ignore the Price Tag
Budget for multiple cycles if needed. Ask about discounts or financing upfront.
Every journey’s unique, so trust your gut and lean on your crew.
The Emotional Side: What They Don’t Tell You
IVF isn’t just needles and labs—it’s a wild ride for your heart too. Couples often talk about the hope-crushing lows (negative tests) and sky-high highs (that first ultrasound). One dad on X shared, “Seeing my wife cry after every failed cycle broke me. But when it worked, we cried harder—for joy.” Research backs this up: a 2019 study found IVF moms and dads often feel more bonded to their kids, maybe because of the struggle to get there.
But it’s not all rosy. Some folks feel guilt or shame if it doesn’t work, like they’ve “failed.” That’s why support groups—online or in-person—are gold. You’re not alone, even when it feels that way.
Checklist: Are You Ready for IVF?
Wondering if IVF’s right for you? Run through this quick list:
- I’ve explored other options (like meds or surgery).
- I’m okay with the cost—or have a plan to cover it.
- I’ve got people to lean on during the ups and downs.
- I’m ready for a process that might take months (or more).
Check off most of these? You’re in a solid spot to start digging deeper.
IVF’s Hidden Challenges: Stuff You Won’t Find in Pamphlets
Most articles gloss over some gritty realities of IVF. Let’s shine a light on three big ones that don’t get enough airtime:
- The Egg Aging Puzzle
As women age, egg quality drops—fast. By 40, only 10-15% of IVF cycles succeed without donor eggs. New research on mitochondrial boosters (like CoQ10) is promising, but it’s not a magic fix yet. It’s a race against time that science is still figuring out. - Implantation Mysteries
Even perfect embryos sometimes don’t stick. Why? The uterus is a picky landlord, and we don’t fully get its rules. A 2007 study called it “the seed, not the soil,” suggesting embryo quality matters more—but the debate’s ongoing. - Male Infertility’s New Frontier
ICSI helps men with low sperm counts, but what about prepubescent boys or transgender women pre-transition? Freezing testicular tissue is in the works, but it’s experimental. This gap leaves some folks out of the IVF club—for now.
These aren’t deal-breakers, but they’re real hurdles that deserve more chatter.
My Take: Why IVF’s Story Matters to You
IVF’s history isn’t just a science tale—it’s a human one. It’s about people like Lesley Brown, who dared to hope, and pioneers like Edwards, who wouldn’t quit. It’s about the 8 million kids who wouldn’t be here without it, and the millions more who might come thanks to what’s next. Whether you’re dreaming of parenthood, curious about science, or just love a good story, IVF’s journey has something for you. It’s proof that when we push boundaries, we don’t just change labs—we change lives.
So, when did IVF begin? Sure, 1978’s the headline, but it’s really a story that stretches back over a century and keeps unfolding every day. What do you think its next chapter will be?