What’s the Difference Between IVF and IUI? A Friendly Guide to Fertility Options
When you’re dreaming of starting a family but things aren’t happening as planned, fertility treatments like IVF and IUI might pop up on your radar. These two options—in vitro fertilization (IVF) and intrauterine insemination (IUI)—are some of the most talked-about ways to help people conceive. But what exactly are they, and how do they differ? If you’re feeling a bit overwhelmed by the jargon or unsure which path might suit you, don’t worry. This guide is here to break it all down in a way that’s easy to grasp, with plenty of real-world insights and a few surprises along the way.
Picture this: IVF and IUI are like two different road trips to the same destination—pregnancy. One’s a scenic, low-key drive, while the other’s a full-on adventure with more stops and detours. By the end of this article, you’ll have a clear map of both journeys, plus some insider tips to help you decide what’s right for you. Let’s dive in!
IVF vs. IUI: The Basics You Need to Know
At their core, IVF and IUI are both fertility treatments designed to give sperm and egg a better shot at meeting up. But the way they make that happen? Totally different. Here’s the quick scoop:
- IUI (Intrauterine Insemination): This is the simpler of the two. Doctors take sperm—either from a partner or a donor—give it a little prep in the lab to boost its quality, and then place it directly into the uterus using a thin tube called a catheter. It’s timed to happen right around ovulation, when an egg is ready to be fertilized. Think of it as giving the sperm a VIP pass to skip the line and get closer to the egg.
- IVF (In Vitro Fertilization): This one’s a bigger production. With IVF, doctors use medications to help a woman’s ovaries produce multiple eggs. Those eggs are then collected in a minor surgery, mixed with sperm in a lab dish (or “in vitro,” which just means “in glass”), and grown into embryos. A few days later, one or two of those embryos are placed back into the uterus to hopefully implant and grow into a baby.
So, in a nutshell: IUI keeps things natural by letting fertilization happen inside the body, while IVF takes the process outside and controls it step-by-step. But there’s so much more to unpack—let’s explore how these treatments work, who they’re for, and what you can expect.
How IUI Works: A Step-by-Step Look
IUI is often the first stop for many people because it’s less invasive and feels a bit more like nature’s way with a little help. Here’s what the process looks like:
- Tracking Ovulation: Timing is everything with IUI. Doctors might monitor your natural cycle using at-home ovulation kits or ultrasound scans to spot when your egg is ready. Sometimes, they’ll give you medications like Clomid or a shot of hCG to trigger ovulation and make sure it happens on schedule.
- Sperm Prep: On the big day, the sperm sample gets “washed” in the lab. This means separating the healthiest, fastest swimmers from the rest of the fluid, so only the best make it to the uterus.
- The Procedure: It’s quick—usually just a few minutes. You lie on an exam table, and the doctor uses a thin catheter to place the sperm directly into your uterus. No anesthesia needed, and most people say it feels like a Pap smear (a little awkward but not painful).
- Waiting Game: After that, you wait about two weeks to take a pregnancy test. The sperm has to swim to the fallopian tube, meet the egg, and fertilize it—all on its own.
Who’s a Good Fit for IUI?
IUI works best for specific situations. It might be right for you if:
- You’re dealing with mild male fertility issues, like low sperm count or slow swimmers.
- You have cervical issues (like thick mucus) that make it hard for sperm to get through naturally.
- You’re a single woman or same-sex couple using donor sperm.
- You’ve got unexplained infertility, and doctors think a little boost could help.
But here’s the catch: IUI needs at least one healthy fallopian tube and decent egg quality. If those aren’t in play, IVF might be the next step.
How IVF Works: The Full Journey
IVF is a bigger commitment—both in time and effort—but it’s also more powerful. Here’s what happens:
- Ovarian Stimulation: For about 10-14 days, you’ll take hormone injections to kick your ovaries into high gear, producing multiple eggs instead of the usual one. You’ll visit the clinic often for ultrasounds and blood tests to check how things are going.
- Egg Retrieval: Once the eggs are ready, doctors retrieve them in a quick procedure under light sedation. A needle guided by ultrasound grabs the eggs from your ovaries—sounds intense, but you’ll be comfy and asleep.
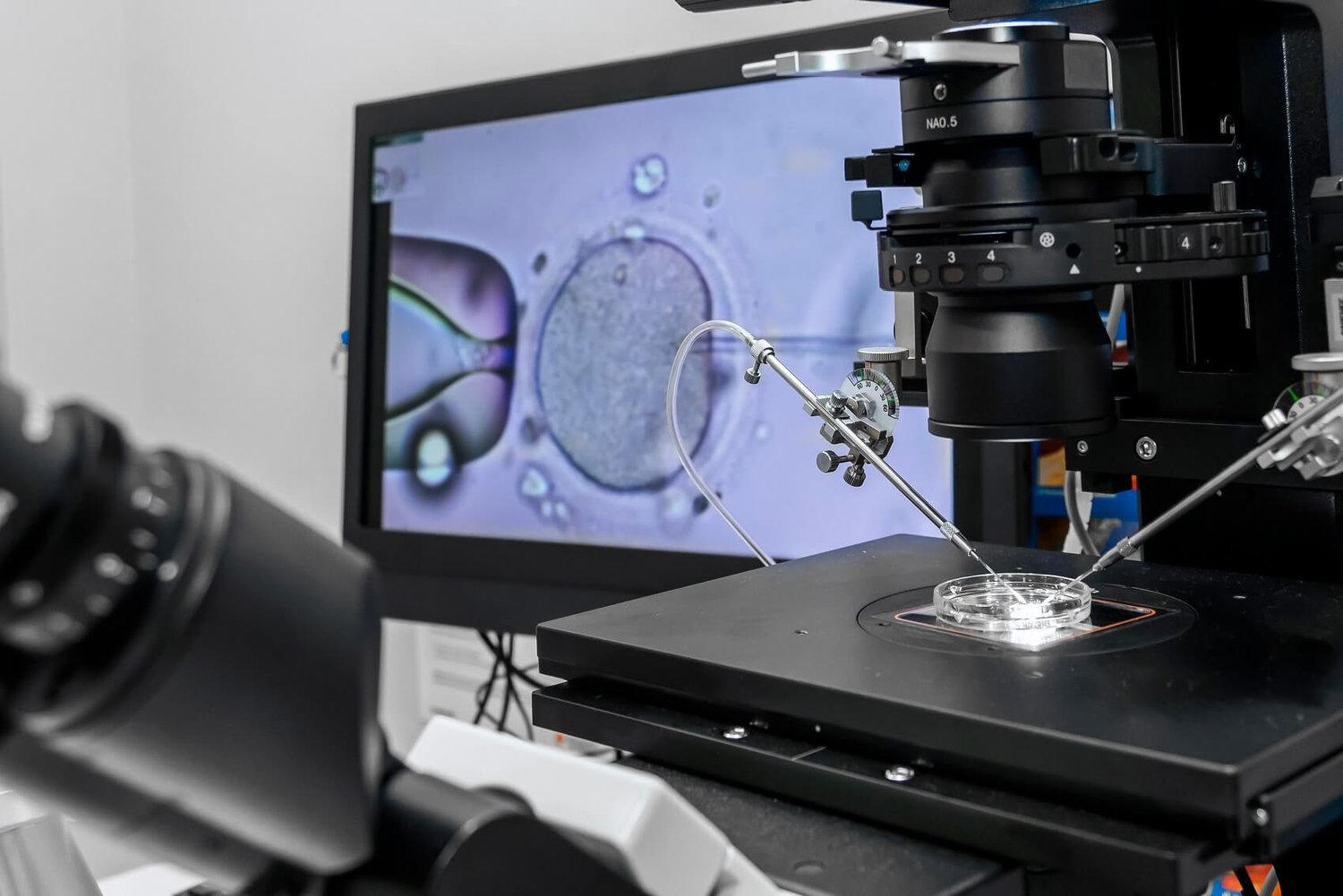
- Fertilization: In the lab, the eggs meet the sperm. Sometimes it’s a simple mix-and-mingle in a dish; other times, a technique called ICSI (intracytoplasmic sperm injection) is used, where a single sperm is injected into an egg for tougher cases.
- Embryo Growth: The fertilized eggs grow into embryos over 3-5 days. Doctors watch them closely to pick the healthiest ones.
- Embryo Transfer: One or two embryos are placed into your uterus using a catheter. It’s painless, like IUI, and you’re awake. Any extra embryos can be frozen for later.
- Waiting for Results: Two weeks later, a blood test tells you if it worked.
Who’s a Good Fit for IVF?
IVF tackles trickier fertility challenges. It might be your go-to if:
- Your fallopian tubes are blocked or damaged.
- You’ve got severe endometriosis or low egg reserves.
- Male infertility is a big factor (like very low sperm count).
- IUI didn’t work after a few tries.
- You want to screen embryos for genetic issues before transfer.
IVF’s flexibility also makes it a favorite for same-sex couples or people using donor eggs, sperm, or surrogates.
Success Rates: What Are Your Chances?
One of the biggest questions people have is, “Will it work?” Success rates depend on a lot—your age, health, and the reason for infertility—but here’s the rundown based on recent data:
- IUI Success Rates: On average, IUI has a 10-20% success rate per cycle for women under 35. That drops to 5-10% for women over 40. It often takes 3-6 tries to see results, and fertility meds can bump those odds up a bit.
- IVF Success Rates: IVF is stronger, with a 40-50% success rate per cycle for women under 35, according to the CDC’s 2021 stats. For women 35-37, it’s around 30-35%, and over 40, it dips to 10-15%. Using younger donor eggs can push those numbers higher.
Why the gap? IVF controls more of the process—doctors pick the best eggs and embryos, and fertilization happens in a lab, not by chance. But success isn’t guaranteed, and both treatments might need multiple rounds.
A Quick Comparison Table
| Factor | IUI | IVF |
|---|---|---|
| Success Rate | 10-20% per cycle | 40-50% per cycle (under 35) |
| Cycles Needed | Often 3-6 | Often 1-2 |
| Age Impact | Drops sharply after 40 | Better odds with donor eggs |
Cost Breakdown: What’s the Price Tag?
Money matters, and these treatments aren’t cheap. Here’s what you’re looking at:
- IUI Costs: A single IUI cycle typically runs $300-$1,000 without insurance, depending on meds and monitoring. Add $500-$1,000 if you’re using donor sperm. It’s affordable upfront, but multiple cycles can add up.
- IVF Costs: IVF is a bigger investment—$12,000-$15,000 per cycle, not counting medications ($3,000-$5,000 more) or extras like genetic testing. Freezing embryos? That’s another $1,000-$2,000, plus storage fees.
Insurance varies wildly. Some states mandate coverage for IUI or IVF, but many don’t. Check your plan, and ask clinics about payment plans or discounts—some offer “shared risk” programs where you get a refund if IVF fails after a set number of tries.
The Emotional and Physical Experience
Fertility treatments aren’t just about science—they’re personal. Here’s what you might feel:
- IUI: Physically, it’s light. You might have mild cramping or bloating from meds, but there’s no surgery. Emotionally, it’s less intense than IVF, but the waiting can still be a rollercoaster. If it fails a few times, frustration can build.
- IVF: The injections and egg retrieval can leave you sore or tired, and hormone swings might make you moody. Emotionally, it’s a marathon—hope, anxiety, and exhaustion all mixed together. But the payoff? Seeing those embryos can feel like a miracle.
Coping Tips
✔️ Lean on a support group—online or in-person—to share the load.
✔️ Plan small treats (a movie night, a walk) to break up the waiting.
❌ Don’t bottle it up—talk to your partner or a friend.
❌ Avoid comparing your journey to others; everyone’s path is unique.
Risks and Realities: What to Watch For
No treatment is risk-free, but knowing what’s possible helps you prepare.
- IUI Risks: Low overall. Fertility drugs might cause ovarian hyperstimulation syndrome (OHSS)—rare, but it can make ovaries swell painfully. There’s also a slight chance of twins (10-15% with meds).
- IVF Risks: Higher stakes. OHSS is more common (1-5% of cases), and multiple pregnancies (twins or more) happen in 20-30% of transfers with two embryos. Egg retrieval carries a tiny risk of bleeding or infection, but it’s rare.
A 2023 study from the Journal of Assisted Reproduction found that single-embryo transfers in IVF cut multiple birth rates without hurting success odds—something to discuss with your doctor if you’re worried about twins.

Three Things You Haven’t Heard About IVF and IUI
Most articles stick to the basics, but here are some fresh angles you won’t find everywhere:
1. The “Hybrid” Option: IUI-to-IVF Conversion
Sometimes, an IVF cycle doesn’t go as planned—say, only a few eggs grow. Instead of canceling, some clinics switch to IUI mid-process, using those eggs naturally. A 2022 study in Fertility and Sterility showed this hybrid approach had a 15% success rate in poor responders, offering a budget-friendly Plan B. Ask your doctor if they’d consider this twist—it’s not widely advertised.
2. Sperm DNA Fragmentation: The Hidden Factor
Success isn’t just about sperm count. Sperm DNA damage—called fragmentation—can tank both IUI and IVF odds, yet it’s rarely tested upfront. A 2024 review in Human Reproduction found that high fragmentation cuts pregnancy rates by 25%. If you’ve had failed cycles, push for this test. Lifestyle tweaks (quitting smoking, eating antioxidants like walnuts) can improve it.
3. The Microbiome Connection
Your uterine microbiome—the bacteria living in there—might play a role in implantation. A 2023 study from Nature Medicine linked a healthy mix of Lactobacillus bacteria to better IVF success. IUI research is lagging, but early data suggests it matters there too. Probiotics or diet changes (more yogurt, less sugar) could be a game-changer—talk to your doc about this cutting-edge idea.
Interactive Quiz: Which Treatment Might Suit You?
Take a quick break and answer these questions (circle your picks):
- How old are you?
A) Under 35
B) 35-40
C) Over 40 - What’s your fertility challenge?
A) Mild sperm issues or unexplained infertility
B) Blocked tubes or severe endometriosis
C) Not sure yet - How much are you willing to spend?
A) Up to $5,000 total
B) $15,000 or more
C) Depends on success odds
Mostly A’s: IUI could be a great starting point—less cost, less stress.
Mostly B’s: IVF might be your best bet for tackling tougher issues.
Mostly C’s: Time to chat with a specialist to narrow it down!
Real Stories: What It’s Like
Numbers are helpful, but stories hit home. Here’s what two people experienced:
- Jess, 32 (IUI): “We tried IUI because my husband’s sperm motility was low. The first two rounds didn’t work, and I was crushed. But the third time, I saw that plus sign. It was simple—no needles, just a quick visit. Totally worth it.”
- Mark, 38 (IVF): “My wife’s tubes were blocked, so IVF was our only shot. The shots were rough, and waiting for the embryo transfer felt endless. When our daughter was born, though, every second was worth it. We even have two frozen embryos left.”
These aren’t one-size-fits-all tales, but they show how personal this choice is.
Making the Decision: Questions to Ask Yourself
Choosing between IVF and IUI isn’t a coin toss—it’s about what fits your life. Here are some prompts to mull over:
- How fast do you want results? IUI’s quicker to start but might take more cycles; IVF’s longer upfront but often faster to success.
- What’s your comfort level? IUI’s low-key; IVF’s more hands-on with meds and procedures.
- What’s your budget? Can you swing IVF’s cost, or is IUI’s price tag more doable?
- What’s your diagnosis? Mild issues lean toward IUI; complex ones point to IVF.
Chat with your partner and doctor too—your team matters as much as the tech.
Boosting Your Odds: Practical Tips for Both
Whether you pick IUI or IVF, little changes can stack the deck in your favor. Here’s how:
✔️ Eat Smart: Load up on fruits, veggies, and healthy fats (think avocado). A 2021 study in Nutrients tied a Mediterranean diet to better IVF outcomes.
✔️ Move More: Light exercise—like yoga or walking—can lower stress and boost blood flow.
✔️ Sleep Well: Aim for 7-8 hours; poor sleep messes with hormones.
❌ Cut Stress: High cortisol can hurt egg quality—try meditation or a hobby.
❌ Skip Alcohol: It’s linked to lower success in both treatments.
The Future of Fertility: What’s Coming?
Fertility tech is evolving fast. Here’s what’s on the horizon:
- AI in IVF: Clinics are using artificial intelligence to pick the best embryos, boosting success rates by 10-15%, per a 2024 Lancet report.
- At-Home Monitoring: New devices let you track ovulation or hormone levels for IUI without tons of clinic visits—convenience is king.
- Gene Editing: Still experimental, but tools like CRISPR could one day fix genetic issues in embryos, making IVF even more precise.
These aren’t here for everyone yet, but they hint at a future where fertility care gets smarter and more tailored.
Poll Time: What’s Your Take?
We’re curious—what’s your biggest concern about fertility treatments? Vote below and see what others think:
- A) Cost
- B) Success rates
- C) Emotional toll
- D) Time commitment
Drop your pick in your mind (or share it with a friend)—it’s a great way to reflect!
Wrapping It Up: Your Next Step
IVF and IUI are like two trusty guides on the road to parenthood—each with its own strengths. IUI’s the gentle nudge, perfect for milder hurdles or a tighter budget. IVF’s the powerhouse, ready to tackle the toughest cases with higher odds. There’s no “better” choice—just the one that fits your story.
If you’re still unsure, start small: book a consult with a fertility specialist. They’ll run tests (like sperm analysis or hormone checks) and map out your options. And hey, you’re not alone—millions have walked this path and found their way.
What’s your gut telling you right now? Whatever it is, trust it—and take that first step when you’re ready. You’ve got this.