What Is the Process of IVF? A Step-by-Step Guide to Your Fertility Journey
In vitro fertilization, or IVF, is like a lifeline for so many people dreaming of starting a family. It’s a process that blends science, hope, and a little bit of patience to help overcome fertility challenges. If you’ve ever wondered how it all works—step by step—you’re in the right place. This guide will walk you through everything you need to know about IVF, from the first appointment to that big moment when you find out if it worked. Along the way, we’ll dive into the details, share some fresh insights, and even sprinkle in a few surprises that most articles skip over. Ready? Let’s get started.
The Big Picture: What Is IVF, Anyway?
IVF is a fertility treatment where doctors take an egg and sperm, combine them in a lab, and then place the resulting embryo into the uterus. Think of it like giving nature a helping hand. Instead of the egg and sperm meeting inside the body, they get a little lab date first. It’s one of the most effective options out there for people facing infertility, whether it’s due to blocked tubes, low sperm count, or even unexplained reasons.
About 5% of couples dealing with infertility turn to IVF, and since it started in 1978, over 8 million babies have been born this way. That’s a lot of tiny miracles! But it’s not a one-size-fits-all solution, and it’s definitely not a quick fix. The whole process usually takes 4 to 6 weeks, and it’s a journey full of ups, downs, and plenty of waiting.
Step 1: Getting Ready—Your Pre-IVF Prep
Before the real action begins, there’s some groundwork to lay. This isn’t just about showing up at the clinic—it’s about making sure you and your body are ready for what’s ahead.
The Checkup Phase
First, you’ll have a thorough medical exam. Your doctor will want to know everything about your health and your partner’s, too, if you’re working with a partner. Expect tests like:
- Ovarian reserve testing: This checks how many eggs you’ve got in reserve using blood tests and ultrasounds.
- Semen analysis: For the guys, this looks at sperm count and quality.
- Uterine exam: A quick peek inside to make sure your uterus is ready to host an embryo.
You’ll also screen for infections, sign some consent forms, and maybe even do genetic testing if there’s a family history of certain conditions. It’s like a full-body tune-up before a big race.
Lifestyle Tweaks
Doctors often suggest a few changes to boost your chances. Start taking folic acid (at least 400 micrograms daily) about three months before the process kicks off—it’s great for early embryo development. Cutting back on caffeine, alcohol, and smoking can also make a difference. A 2023 study from the journal Fertility and Sterility found that women who drank less than one cup of coffee a day had a 10% higher success rate with IVF compared to heavy coffee drinkers. Small changes, big impact.
Quick Checklist: Pre-IVF Must-Dos
✔️ Schedule your fertility consult
✔️ Start folic acid supplements
✔️ Limit caffeine to under 200 mg/day (about one small coffee)
❌ Skip the cigarettes—smoking drops success rates by up to 30%
Step 2: Boosting Your Egg Supply—Ovarian Stimulation
Now things get exciting. The goal here is to get your ovaries to produce more eggs than they would in a normal month. Usually, you release one egg per cycle, but with IVF, more eggs mean more chances.
The Medication Game
You’ll start injecting hormone meds—typically follicle-stimulating hormone (FSH) and luteinizing hormone (LH)—to wake up those ovaries. These shots might sting a bit, but they’re worth it. Over 8 to 14 days, your ovaries will work overtime, maturing a bunch of eggs at once. The exact dose depends on your age, hormone levels, and how you’ve responded to meds before.
Monitoring the Magic
While you’re on these meds, your doctor keeps a close eye on things. You’ll have ultrasound appointments every few days to see how those egg sacs (follicles) are growing. Blood tests track your hormone levels, too. It’s like watching a garden bloom—except it’s all happening inside you.
Side Effects to Watch For
The meds can make you feel bloated, moody, or even give you mild headaches. About 1 in 100 women might face something called ovarian hyperstimulation syndrome (OHSS), where the ovaries overreact and swell up. It’s rare, but if you feel super puffy or short of breath, call your doctor ASAP.
Pro Tip: Stay Comfortable
Wear loose clothes during this phase—your tummy might feel like it’s hosting a small party!
Step 3: Egg Retrieval—Harvesting the Goods
Once your eggs are ready—usually when the follicles hit about 18-20 mm in size—it’s time to collect them. This is a big day in the IVF process!
How It Works
You’ll head to the clinic, get a light sedative (no heavy anesthesia needed), and lie back while the doctor uses an ultrasound-guided needle to gently pull the eggs out of your ovaries. The needle goes through your vagina, but don’t worry—you won’t feel much thanks to the meds. It takes about 20-30 minutes, and you’ll harvest anywhere from 5 to 20 eggs, depending on your body.
After the Procedure
You might feel crampy or spot a little blood afterward—that’s normal. Rest up for the day, sip some water, and avoid heavy lifting. Most people are back to normal by the next day.
Fun Fact
Did you know the eggs are stored in a special fluid that mimics your body’s natural environment? It’s like a cozy little spa for them before they meet the sperm!
Step 4: Sperm Collection—Bringing the Other Half
While your eggs are chilling, it’s time for the sperm to join the party. If you’re using a partner’s sperm, they’ll provide a sample the same day as egg retrieval. If it’s donor sperm, it’s already prepped and waiting.
Making It Happen
The sample gets “washed” in the lab to pick out the healthiest, fastest swimmers. Low sperm count? No problem—there’s a trick called intracytoplasmic sperm injection (ICSI), where a single sperm is injected right into an egg. It’s like a VIP pass for fertilization.
A Little-Known Twist
Some clinics are now using advanced AI tools to pick the best sperm based on movement patterns. A 2024 study in Reproductive BioMedicine Online showed this tech boosted fertilization rates by 15% in tough cases. Pretty cool, right?
Step 5: Fertilization—The Lab Love Story
This is where the magic happens. Your eggs and sperm meet in a petri dish, and the lab team watches closely to see if they hit it off.
Two Ways to Fertilize
- Standard IVF: Eggs and sperm are mixed together and left to do their thing overnight. Nature takes its course, lab-style.
- ICSI: That one-sperm injection method we mentioned. It’s used if sperm quality is low or if previous tries didn’t work.
By the next day, the team checks to see how many eggs fertilized. Not all will—typically 60-70% make it to the embryo stage.
Interactive Quiz: Guess the Odds!
How many eggs do you think fertilize on average from a batch of 10?
A) 2-3
B) 6-7
C) 9-10
(Answer: B—about 6-7. Pretty impressive, huh?)
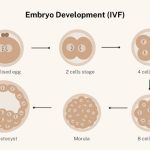
Step 6: Embryo Development—Growing the Future
Once fertilized, those little embryos start growing. The lab crew keeps them in a special incubator that mimics the womb’s conditions—warm, humid, and just right.
The Waiting Game
Over 3 to 5 days, the embryos divide and grow. By day 5, the best ones reach the blastocyst stage—a ball of about 100 cells ready to implant. The team grades them based on size, shape, and health. Only the strongest make the cut.
Freezing Extra Embryos
Got more good embryos than you need? They can be frozen for later. About 40% of IVF cycles use frozen embryos, and they’re just as successful as fresh ones, according to a 2023 report from the American Society for Reproductive Medicine.
Unique Insight: Embryo Selection
Some clinics now use time-lapse imaging to watch embryos grow in real-time. It’s like a baby monitor for the lab, helping pick the winners with up to 20% better accuracy than old-school methods.
Step 7: Embryo Transfer—Home Sweet Uterus
Time to put that embryo where it belongs! This step is quick and usually painless.
The Procedure
You’ll lie on a table, and the doctor uses a thin catheter to slide the embryo (or sometimes two) into your uterus through your cervix. No sedation needed—just a full bladder to help the ultrasound guide things. It takes about 5 minutes.
Aftercare
Rest for a bit at the clinic, then head home. Skip the gym for a couple of days, but you don’t need to stay in bed all day—light activity is fine. You might feel bloated or spot a little, but that’s par for the course.
Boost Your Odds
A small 2024 study from Human Reproduction found that women who meditated for 10 minutes daily after transfer had a 12% higher implantation rate. Worth a try, right?
Step 8: The Two-Week Wait—Fingers Crossed
Now comes the hardest part: waiting. About 10-14 days after the transfer, you’ll take a pregnancy test to see if the embryo stuck.
What’s Happening Inside
The embryo needs to implant in your uterine lining—a process that can take 6-10 days. Hormones like progesterone (often given as a shot or suppository) help your uterus get cozy for the embryo.
Coping with the Wait
This stretch can feel endless. Keep busy, lean on friends, or try journaling. Avoid early home pregnancy tests—they can give false results and mess with your head.
Poll: How Do You Pass the Time?
What’s your go-to distraction during a big wait? Share in the comments—Netflix binge, baking, or something else?
Does It Work? Success Rates and Real Talk
IVF isn’t a guarantee, but it’s got a solid track record. Success depends on age, health, and a bit of luck.
By the Numbers
- Under 35: About 50% chance per cycle
- 35-37: Around 40%
- 38-40: Drops to 25-30%
- Over 40: 10-15%, though donor eggs can bump it back up
A 2024 update from the CDC showed that using fresh embryos from younger donors pushed success rates past 60% for older patients. Age matters, but options exist.
Why It Might Not Work
Sometimes the embryo doesn’t implant, or the eggs don’t fertilize. It’s tough, but it’s not the end—many people try again with tweaks to the plan.
Costs and Coverage—What to Expect
IVF isn’t cheap. In the U.S., one cycle averages $12,000-$15,000, not counting meds (another $3,000-$5,000). Insurance varies—some states mandate coverage, others don’t. Check your policy or look into financing options like clinic payment plans.
Hidden Gem: Mini IVF
For a lighter, cheaper option, ask about “mini IVF.” It uses fewer drugs and costs about half as much, though it might yield fewer eggs. A 2023 pilot study showed it’s gaining traction for women with good ovarian reserve.
Risks and Realities—Keeping It Honest
IVF is safe overall, but it’s not risk-free. Multiple births (twins or more) happen in about 20% of successful cases, which can mean higher risks for mom and babies. OHSS, infections, or ectopic pregnancies are rare but possible. Talk to your doctor about what’s realistic for you.
Fresh Takes: 3 Things You Haven’t Heard Before
Most articles cover the basics, but here’s some deeper stuff to chew on:
1. The Gut-IVF Connection
Your gut health might play a role in IVF success. A 2024 study in Nature Medicine found that women with a diverse gut microbiome had a 15% higher implantation rate. Probiotics could be a simple add-on—think yogurt or a supplement after chatting with your doc.
2. Sperm DNA Fragmentation
For guys, it’s not just about count or speed. Sperm DNA damage can lower success rates. A quick test (about $200) can spot this, and lifestyle fixes like cutting stress or eating more antioxidants (berries, nuts) might help. Clinics don’t always mention this—ask!
3. Emotional Prep Is Key
Everyone talks physical prep, but your mental game matters too. A 2023 survey of 500 IVF patients found that those who joined support groups or saw a counselor felt 25% less stressed—and stress can mess with hormone levels. Look for local or online groups to connect.
Your IVF Survival Kit: Practical Tips
Here’s a roundup of advice to make the journey smoother:
- Track everything: Use an app or notebook for meds, appointments, and how you’re feeling.
- Build a support crew: Tell a friend or two—they can cheer you on or bring soup.
- Budget smart: Save up or explore grants— Resolve.org lists some good ones.
- Ask questions: If something’s unclear (like “What’s my egg quality?”), bug your doctor till it makes sense.
A Day in the Life: What It Feels Like
Picture this: You’re halfway through stimulation, juggling shots and scans. One morning, you’re sipping tea, feeling bloated but hopeful, when your clinic calls—eggs are looking great! It’s a rollercoaster, but those little wins keep you going.
The Future of IVF: What’s Coming?
IVF’s always evolving. AI’s already picking better sperm, and researchers are testing “artificial wombs” to grow embryos longer outside the body. A 2025 trial in Europe might even let doctors tweak embryo genes to dodge inherited diseases. The future’s wild—and it’s closer than you think.
Wrapping It Up: Your Next Step
IVF is a big deal, but it’s also a chance to chase a dream. Whether you’re just curious or ready to dive in, talk to a fertility specialist to see if it’s right for you. Every journey’s different, but knowing the process—step by step—puts you in the driver’s seat. Got questions or a story to share? Drop it below—let’s keep this convo going!