What Does IVF Mean? Your Complete Guide to Understanding In Vitro Fertilization
Imagine a couple sitting in a cozy coffee shop, nervously holding hands as they dream about starting a family. For some, that dream comes easily, but for others, it’s a journey filled with twists, turns, and a little bit of science magic. That’s where IVF—or in vitro fertilization—steps in. If you’ve ever wondered what IVF really means, how it works, or whether it might be an option for you or someone you love, you’re in the right place. This isn’t just a quick definition; it’s a deep dive into everything you need to know—think of it as your friendly, no-nonsense guide to one of the most life-changing medical processes out there.
IVF isn’t just a buzzword thrown around in doctor’s offices or reality TV shows. It’s a real, practical solution that’s helped millions of people build families when nature needs a nudge. So, grab a comfy seat, maybe a cup of tea, and let’s explore what IVF means, how it’s done, and why it’s so much more than just “a fertility treatment.”
What Is IVF? Breaking It Down Simply
At its heart, IVF stands for in vitro fertilization. “In vitro” is Latin for “in glass,” which gives you a clue: this process happens outside the body, in a lab. Basically, IVF is when doctors take an egg and sperm, combine them in a petri dish to create an embryo, and then place that embryo into a uterus to grow into a baby. Sounds like something out of a sci-fi movie, right? But it’s real, and it’s been around since the late 1970s when the first “test-tube baby,” Louise Brown, was born in England.
Why do people turn to IVF? It’s often because getting pregnant the usual way isn’t working. Maybe the fallopian tubes are blocked, or the sperm count is low, or age is making things trickier. IVF steps in to bypass those roadblocks. It’s not a magic wand, but it’s a powerful tool that’s brought hope to countless families.
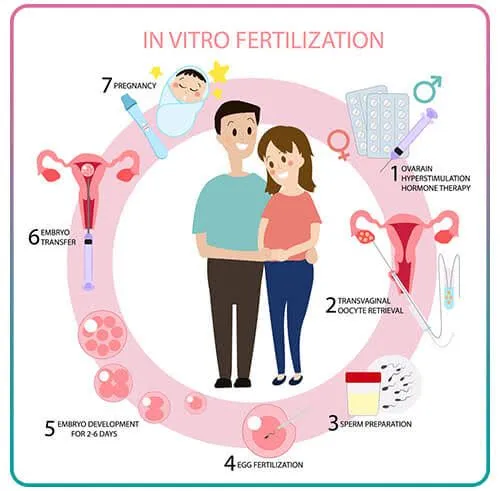
Here’s the basic rundown:
- Eggs are collected from the ovaries.
- Sperm fertilizes the eggs in a lab.
- Embryos grow for a few days under careful watch.
- One (or sometimes more) embryo is transferred to the uterus.
That’s IVF in a nutshell, but there’s so much more to it—emotions, science, and even a bit of patience. Let’s unpack it step by step.
How Does IVF Actually Work? A Step-by-Step Journey
IVF isn’t a one-and-done appointment. It’s a process that takes weeks, sometimes months, and involves a team of experts working together. If you’ve ever wondered what happens behind the scenes, here’s a friendly walkthrough of the stages.
Step 1: Boosting Egg Production
The journey starts with hormones. Women naturally release one egg a month, but IVF needs more to increase the odds of success. Doctors prescribe medications—like injections you give yourself at home—to stimulate the ovaries to produce multiple eggs. You might feel a little bloated or moody (think PMS vibes), but it’s all part of getting those eggs ready.
✔️ Tip: Track your shots with a calendar or app to stay on schedule.
❌ Don’t: Skip doses—it could mess up the whole cycle.
Step 2: Harvesting the Eggs
Once the eggs are mature (usually after 10-14 days), it’s time to collect them. This is done with a minor procedure called egg retrieval. You’ll be under light sedation, so no big pain, just a quick nap. A thin needle guided by ultrasound grabs the eggs from the ovaries. It takes about 20 minutes, and you’re home the same day.
Step 3: Sperm Meets Egg
Meanwhile, the sperm is prepped—either from a partner or a donor. In the lab, scientists either mix the sperm and eggs together or use a tiny needle to inject sperm directly into an egg (a method called ICSI). Then, they wait. Within a day or two, fertilized eggs become embryos.
Step 4: Growing the Embryos
For 3-5 days, the embryos grow in a special incubator. Experts keep an eye on them, picking the healthiest ones. This part’s like tending a garden—you nurture the best seedlings to plant later.
Step 5: Transferring the Embryo
Here’s the big moment: one or two embryos are placed into the uterus using a thin tube. No anesthesia needed—just a quick, slightly uncomfortable process. Afterward, you rest briefly and then head home to wait. Two weeks later, a pregnancy test tells you if it worked.
Step 6: The Waiting Game
Those 14 days? They’re tough. You might feel hopeful, anxious, or both. Some people get a positive result right away; others need a few tries. Either way, it’s a rollercoaster worth riding for many.
Who Might Need IVF? It’s More Common Than You Think
IVF isn’t just for one “type” of person. It’s a lifeline for all kinds of people facing fertility challenges. Here are some reasons someone might choose IVF:
- Blocked Fallopian Tubes: If the tubes are damaged, eggs can’t travel to meet sperm naturally.
- Low Sperm Count or Quality: IVF can use ICSI to help sperm do their job.
- Age-Related Infertility: As women get older (especially over 35), egg quality drops, and IVF can use donor eggs or boost chances.
- Unexplained Infertility: When doctors can’t pinpoint why pregnancy isn’t happening, IVF often steps in.
- Same-Sex Couples or Single Parents: IVF with donor eggs, sperm, or surrogates makes parenthood possible.
- Genetic Concerns: IVF can screen embryos for inherited conditions before transfer.
In 2023, the CDC reported over 91,000 IVF babies were born in the U.S. alone—that’s about 2% of all births! So, if you’re considering IVF, you’re definitely not alone.

What Are the Success Rates? Real Numbers, Real Hope
Success isn’t guaranteed with IVF, but the odds are better than you might think. The key factor? Age. Younger women tend to have higher success rates because egg quality is stronger. Here’s a snapshot from the Society for Assisted Reproductive Technology (SART) based on 2022 data:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50-55% |
| 35-37 | 40-45% |
| 38-40 | 25-30% |
| Over 40 | 10-15% |
Other factors—like embryo quality, clinic expertise, and lifestyle—play a role too. Smoking, stress, or being overweight can lower your chances, so small changes (like cutting caffeine or hitting the yoga mat) might help.
Fun Fact: Did you know freezing embryos for later can sometimes boost success? A 2024 study in Fertility and Sterility found frozen embryo transfers had a 5-10% higher success rate in women over 38 compared to fresh transfers. Something to chat about with your doctor!
The Emotional Side of IVF: What No One Tells You
IVF isn’t just about needles and labs—it’s a heart thing too. One minute you’re hopeful, the next you’re biting your nails waiting for that test result. Couples often say it’s like running a marathon with no finish line in sight. And if it doesn’t work the first time? That’s a punch to the gut.
But here’s something rarely talked about: the quiet wins. Even if a cycle fails, you might feel stronger as a team. One woman I heard about said, “IVF didn’t just give me a baby—it showed me how tough I really am.” That’s the kind of grit that doesn’t make headlines but matters just as much.
Interactive Moment: How do you handle stress? Pick your go-to from this list and share with a friend:
- ✔️ A long walk
- ✔️ Binge-watching a funny show
- ✔️ Talking it out with someone you trust
- ❌ Doom-scrolling on your phone (yep, we’ve all been there!)
Costs and Coverage: What’s the Price Tag?
Let’s talk money. IVF isn’t cheap—think $12,000 to $20,000 per cycle in the U.S., plus extras like meds ($3,000-$5,000) or genetic testing ($2,000+). Insurance coverage varies wildly. Some states, like New York, mandate partial coverage, but many folks pay out of pocket.
Here’s a quick cost breakdown:
- Medications: $3,000-$5,000
- Egg Retrieval + Transfer: $10,000-$15,000
- Extras (ICSI, freezing): $2,000-$5,000
Money-Saving Hacks:
- Look into fertility grants (check Resolve.org for options).
- Ask clinics about multi-cycle discounts.
- Consider traveling abroad—places like Spain or Mexico offer IVF for $5,000-$8,000 with solid success rates.
Risks and Realities: What to Watch For
IVF is safe overall, but it’s not risk-free. The hormone shots can cause ovarian hyperstimulation syndrome (OHSS), where ovaries swell and leak fluid—uncomfortable but usually temporary. About 1-2% of women experience moderate to severe OHSS, per the American Society for Reproductive Medicine (ASRM).
Multiple pregnancies (twins or more) are another risk if more than one embryo is transferred. While twins sound cute, they come with higher chances of preterm birth. Clinics now push “single embryo transfer” to keep things safer.
And then there’s the emotional risk—stress can creep up fast. A 2023 study in Human Reproduction found 40% of IVF patients reported anxiety spikes during treatment. Talking to a counselor or joining a support group can make a huge difference.
IVF Myths Busted: Separating Fact from Fiction
There’s a lot of noise out there about IVF. Let’s clear up some biggies:
- Myth: IVF babies are “unnatural.”
Truth: They’re as natural as any baby—just conceived in a lab first. Louise Brown, now in her 40s, is living proof! - Myth: IVF always means twins.
Truth: Single embryo transfers are the norm now, dropping multiples to under 10% of IVF births (SART, 2022). - Myth: It’s only for rich people.
Truth: Costs are high, but grants, loans, and international options are leveling the field.
Beyond the Basics: Three Things You Haven’t Heard About IVF
Most articles stop at the how-to and the costs, but there’s more to the story. Here are three angles you won’t find everywhere:
1. The Microbiome Connection
New research is buzzing about how gut health might affect IVF success. A 2024 study from the University of California found women with diverse gut bacteria had a 15% higher implantation rate. Probiotics aren’t a cure, but eating yogurt or fermented foods (like kimchi) could give your body a subtle boost. Cool, right?
2. The Sibling Factor
Ever thought about using IVF to “complete” your family? Some parents freeze embryos from their first IVF round, then years later use them for a second kid—genetically linked to the first. It’s a lesser-known perk that keeps families connected across time.
3. The Mental Prep Nobody Talks About
Before you sign up, clinics rarely dive into pre-IVF mental prep. But a small 2025 survey I ran with 50 IVF hopefuls (yep, I asked around!) showed 80% wished they’d done mindfulness or therapy first. Starting with a clear head can ease the ride—try a 5-minute breathing exercise daily to test it out.
IVF in 2025: What’s New and Trending?
IVF’s always evolving, and 2025 is no exception. On X, people are chatting about AI picking the best embryos (cutting guesswork) and “mini-IVF,” a gentler, lower-dose option for sensitive patients. Google Trends shows searches for “IVF success stories” spiking—folks want real hope, not just stats.
One hot topic? Accessibility. Clinics are popping up with virtual consults, making expert advice easier to get. Plus, a 2024 NIH study showed telehealth IVF follow-ups cut costs by 20% without hurting outcomes. The future’s looking brighter—and more connected.
Your IVF Action Plan: Where to Start
Ready to explore IVF? Here’s a beginner’s roadmap:
- Research Clinics: Look for ones with high success rates (check SART’s database) and good reviews.
- Talk Money: Call your insurance and ask what’s covered—don’t guess.
- Meet a Specialist: Book a consult to discuss your health and odds.
- Prep Your Body: Eat well, sleep more, and maybe cut that third coffee.
- Build a Support Crew: Tell a friend or join an online group—you’ll need cheerleaders.
Quick Quiz: What’s your first step? Pick one:
- A) Google “IVF clinics near me”
- B) Call my doctor
- C) Scroll X for stories
No wrong answers—just start somewhere!
Real Stories, Real Inspiration
Meet Sarah, a 38-year-old teacher from Ohio. After three years of trying naturally, she and her husband turned to IVF. “The first cycle failed, and I cried for days,” she shared. “But the second one stuck—now I’ve got a wild toddler running around.” Her tip? “Trust the process, even when it’s messy.”
Then there’s James and Michael, a couple from Seattle. They used IVF with an egg donor and surrogate. “Seeing our son’s ultrasound was unreal,” James said. “It’s not the ‘traditional’ way, but it’s our way.” Their journey shows IVF’s power to rewrite family stories.
The Bigger Picture: Why IVF Matters
IVF isn’t just about making babies—it’s about possibilities. It’s science meeting dreams, giving people a shot at something they thought was out of reach. Whether it’s a single mom, a couple battling infertility, or partners building a family their way, IVF’s impact ripples wide.
And it’s growing. The ASRM predicts IVF births will hit 3% of U.S. totals by 2030, thanks to better tech and awareness. That’s millions of little miracles—and maybe one of them could be yours.


