How Many Embryos Are Used in IVF? Your Guide to Understanding the Numbers
In vitro fertilization (IVF) is a life-changing journey for many hopeful parents. It’s a process filled with hope, science, and a sprinkle of wonder—but also plenty of questions. One that pops up a lot is: How many embryos are involved in IVF? Whether you’re just starting to explore fertility treatments or you’re knee-deep in the process, understanding the numbers behind embryos can feel like cracking a code. Don’t worry—I’ve got you covered with a deep dive into this topic that’s packed with insights, practical tips, and even a few surprises most articles skip over.
From how many eggs turn into embryos to how many get transferred into the womb, we’ll walk through it all step-by-step. Plus, I’ll share some fresh angles—like what happens to unused embryos and how new research is shaking things up. So, grab a cozy drink, settle in, and let’s unpack the world of IVF embryos together!
What Happens Before Embryos Even Exist?
IVF doesn’t start with embryos—it starts with eggs. To get there, doctors use a carefully planned process called ovarian stimulation. Think of it like giving your ovaries a pep talk to produce more eggs than they would in a natural cycle (usually just one). Here’s how it works:
- Hormone Boost: You’ll take medications (like follicle-stimulating hormone, or FSH) for about 10-14 days to encourage your ovaries to grow multiple eggs.
- Monitoring: Doctors keep a close eye on your progress with ultrasounds and blood tests to see how many follicles (egg-containing sacs) are developing.
- Egg Retrieval: Once the follicles are ready, a quick procedure collects the eggs—usually 8-15, though this varies widely based on age, health, and response to meds.
Now, not every egg retrieved is a winner. Some might not be mature enough to fertilize, and others might not survive the next step. On average, about 70-80% of retrieved eggs are mature and ready to meet some sperm. That’s where the embryo journey really begins.
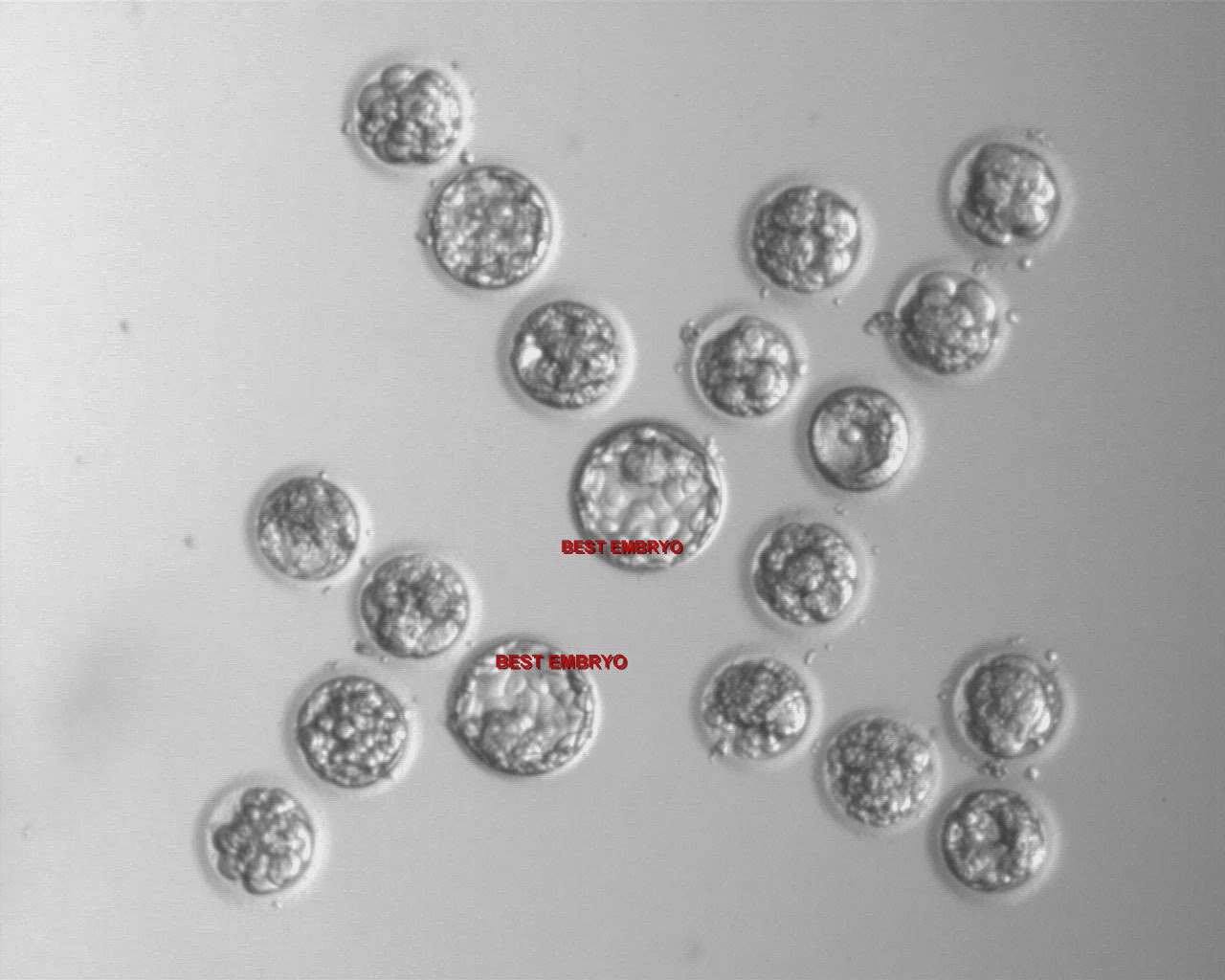
How Many Eggs Become Embryos?
Once the eggs are collected, it’s time for fertilization. This can happen in two ways: traditional IVF (where eggs and sperm hang out together in a dish) or intracytoplasmic sperm injection (ICSI), where a single sperm is injected into each egg. But here’s the catch—not every egg turns into an embryo.
- Fertilization Rate: Studies show that about 60-70% of mature eggs successfully fertilize. So, if 10 eggs are retrieved and 8 are mature, you might end up with 5-6 embryos.
- Quality Matters: Even fertilized eggs don’t always grow into healthy embryos. Some stop developing early, leaving you with fewer viable ones by day 3 or 5 of growth.
For example, imagine starting with 12 eggs. After retrieval, 10 might be mature, and 7 could fertilize. By day 5, when embryos reach the blastocyst stage (a key milestone), you might be down to 4 or 5 strong contenders. It’s a bit like a talent show—only the best make it to the final round!
Why Do Some Embryos Drop Out?
- Chromosomal Issues: Many embryos have genetic abnormalities that stop them from growing, especially as women get older.
- Lab Conditions: Even with top-notch labs, tiny differences in environment can affect development.
- Natural Selection: Some embryos just aren’t meant to thrive—it’s nature’s way of filtering.
This “dropout rate” is totally normal, but it’s why doctors aim to start with more eggs—to increase the odds of getting at least one healthy embryo.
How Many Embryos Are Transferred in IVF?
Here’s where things get personal. The number of embryos transferred into the womb isn’t a one-size-fits-all decision—it depends on your age, health, and goals. Doctors usually aim to balance success rates with safety, avoiding multiples (like twins or triplets) that can raise risks for mom and babies.
The Numbers Game
- Under 35: Often 1 embryo, sometimes 2 if quality or past cycles suggest it’s needed.
- 35-40: 1-2 embryos, depending on embryo quality and history.
- Over 40: 2-3 embryos might be considered, especially if using your own eggs, since success rates drop with age.
In 2021, the Human Fertilisation and Embryology Authority (HFEA) in the UK reported that 75% of IVF cycles used a single embryo transfer (SET)—a big jump from just 13% in 1991. Why? Better lab techniques mean one high-quality embryo can do the job, and it cuts the chance of multiples (down to 4% in 2022 from 28% decades ago).
Fresh vs. Frozen Transfers
- Fresh Transfer: Embryos go into the womb 3-5 days after retrieval. You might transfer 1-2, depending on how many look promising.
- Frozen Transfer: Extra embryos are frozen, and later cycles might use 1 at a time. Frozen transfers are on the rise—up 86% from 2014 to 2019—because they often have higher success rates.
Real-Life Example
Take Sarah, 32, who had 10 eggs retrieved. Seven fertilized, and by day 5, she had 3 blastocysts. Her doctor suggested transferring 1 fresh embryo and freezing the rest. It worked—she’s now a mom! The frozen ones are her backup plan for baby #2.
What Happens to Extra Embryos?
Not every embryo gets transferred right away, so what happens to the leftovers? This is a big question that doesn’t get enough airtime, and it’s worth exploring.
- Freezing: Most extras are cryopreserved (frozen) for future use. About 30-40% of IVF births now come from frozen embryos, thanks to improved freezing tech like vitrification.
- Donation: Some families donate unused embryos to other couples or for research—about 2-3% of embryos in the U.S. take this path.
- Discarding: If you’re done building your family, embryos can be discarded. It’s a tough call, but it happens more than you’d think—up to 20% of IVF patients opt for this.
The Emotional Side
Deciding what to do with extra embryos can feel overwhelming. One couple I heard about froze 5 embryos after their first child was born. Years later, they debated donating them but chose to keep them “just in case.” It’s a personal choice, and clinics often offer counseling to help.
Success Rates: How Many Embryos Make It?
Success in IVF isn’t just about how many embryos you start with—it’s about how many lead to a baby. Here’s the scoop:
- Implantation Rate: About 25-30% of transferred embryos implant in the uterus per cycle, per the American Society for Reproductive Medicine (ASRM).
- Live Birth Rate: For women under 35, it’s around 32% per embryo transferred (HFEA, 2021). Over 43? It drops to 4-5% with your own eggs.
Fun Fact
Natural conception has a higher embryo loss rate—70-85% don’t implant—compared to IVF’s 70% failure rate. IVF’s controlled process actually gives embryos a better shot!
Interactive Quiz: What’s Your IVF Number?
Curious how many embryos you might get? Try this quick quiz:
- How old are you?
- A) Under 35
- B) 35-40
- C) Over 40
- How many eggs do you think you’d retrieve?
- A) 5-10
- B) 10-15
- C) 15+
- Are you open to freezing extras?
- A) Yes
- B) No
Results:
- Mostly A’s: You might start with 3-5 strong embryos, with 1-2 transferred.
- Mostly B’s: Expect 5-8 embryos, with flexibility for freezing.
- Mostly C’s: Could be 8+ embryos, but age might trim the viable ones.
This is just a fun guess—talk to your doctor for the real deal!
New Research: Changing the Embryo Game
IVF isn’t standing still. Recent studies are flipping the script on how many embryos we need and how we use them. Here are three breakthroughs you won’t find in most articles:
1. Fewer Eggs, Better Outcomes?
A 2023 study from the University of Colorado found that retrieving fewer eggs (5-8) with gentler stimulation can still yield 1-2 top-quality embryos—enough for success without overloading your system. It’s called “mild IVF,” and it’s gaining fans for being less stressful and cheaper.
2. AI Picks the Winners
Artificial intelligence is stepping in to predict which embryos will thrive. A 2024 trial in Europe showed AI boosting implantation rates by 15% by analyzing embryo images. Fewer embryos transferred, higher success—pretty cool, right?
3. Lab-Grown Embryos?
Scientists are now growing embryo-like structures from stem cells (not real embryos, but close). A 2022 paper in Nature suggests this could one day cut the need for multiple egg retrievals, though it’s years from clinical use. Imagine needing just one egg to create endless possibilities!

How to Maximize Your Embryo Count
Want to boost your chances of getting more healthy embryos? Here are some practical tips groundedadoras://i.imgur.com/k4r5x9y.png
Before IVF
- Eat Smart: Load up on antioxidants (berries, nuts) and protein (eggs, fish) to support egg quality.
- Cut Stress: Yoga or meditation can lower cortisol, which might help your ovaries respond better.
- Sleep Well: Aim for 7-9 hours—poor sleep messes with hormones.
During IVF
- Ask About Protocols: Mild stimulation might mean fewer eggs but better quality.
- Consider PGT-A: Preimplantation genetic testing can spot chromosomal winners, upping your odds.
- Freeze Early: Freezing all embryos (not transferring fresh) can let your body recover, improving implantation chances.
Common Myths About Embryo Numbers
Let’s bust some myths floating around:
- ❌ More embryos transferred = higher success. Nope—after 1-2, extra embryos just raise multiple risks, not birth rates.
- ❌ IVF always makes tons of embryos. Not true—some folks get just 1 or 2, and that’s okay!
- ✔️ Frozen embryos are just as good. Actually, they’re often better—success rates are climbing.
What If You Don’t Get Enough Embryos?
Sometimes, the numbers don’t add up—maybe you only get 1 embryo, or none make it to blastocyst. It’s tough, but not the end:
- Try Again: A new cycle with adjusted meds might yield more.
- Donor Eggs: If age is the issue, donor eggs often mean more embryos (and higher success—over 30% across ages).
- Embryo Pooling: Do multiple retrievals, freeze embryos, then transfer later.
Take Lisa, 41, who got 2 embryos in her first cycle—neither worked. She switched to donor eggs, got 6 embryos, and welcomed twins. Options exist—don’t lose hope!
The Big Picture: Embryo Numbers Over Time
IVF has evolved big-time. Back in 1978, Louise Brown (the first IVF baby) came from 1 egg, no extras. Today, we’re averaging 5-10 embryos per cycle, with freezing and single transfers as the norm. By 2030, experts predict AI and stem-cell tech could shrink those numbers while boosting success—fewer embryos, better outcomes.
Quick Stat
In 1991, IVF birth rates were 7% per embryo for 35-37-year-olds. By 2021, it’s 25%. Progress rocks!
Your IVF Embryo Journey: What to Expect
Every IVF story is unique, but here’s a rough timeline:
- Stimulation (10-14 days): Eggs grow, monitored closely.
- Retrieval (Day 0): Eggs collected—aim for 8-15.
- Fertilization (Day 1): Eggs meet sperm; 60-70% fertilize.
- Growth (Days 3-5): Embryos develop—3-5 might reach blastocyst.
- Transfer or Freeze: 1-2 go in, extras get stored.
Poll: How Many Embryos Do You Hope For?
- 1-2: Happy with a couple of stars.
- 3-5: A solid lineup.
- 6+: Bring on the reserves!
Drop your vote in your head—or share with a friend!

