How Far Along Am I in IVF? Your Guide to Tracking Your Journey
Starting an IVF journey is like stepping onto a roller coaster—exciting, nerve-wracking, and full of twists and turns. If you’re here, you’re probably wondering, “How far along am I in IVF?” Maybe you’re counting the days since your last injection, or you’re curious about what’s happening inside your body right now. Don’t worry—you’re not alone! This guide is your roadmap to understanding where you are in the process, what to expect next, and how to feel more in control of this wild ride.
IVF (in vitro fertilization) can feel overwhelming with all its stages, timelines, and medical terms. But breaking it down into bite-sized pieces makes it easier to see where you fit in. Whether you’re just starting stimulation meds or anxiously awaiting a pregnancy test, we’ve got you covered with practical tips, the latest research, and some fresh insights you won’t find everywhere else. Let’s dive in and figure out exactly where you are—and what’s coming up!
What Is IVF and How Does It Work?
IVF is a fertility treatment where doctors help create a baby by combining eggs and sperm outside the body, then placing the resulting embryo into the uterus. It’s a process that’s helped millions of people build families, but it’s not a one-day deal—it’s a series of steps that can take weeks or even months. Knowing the big picture can help you pinpoint your spot in the timeline.
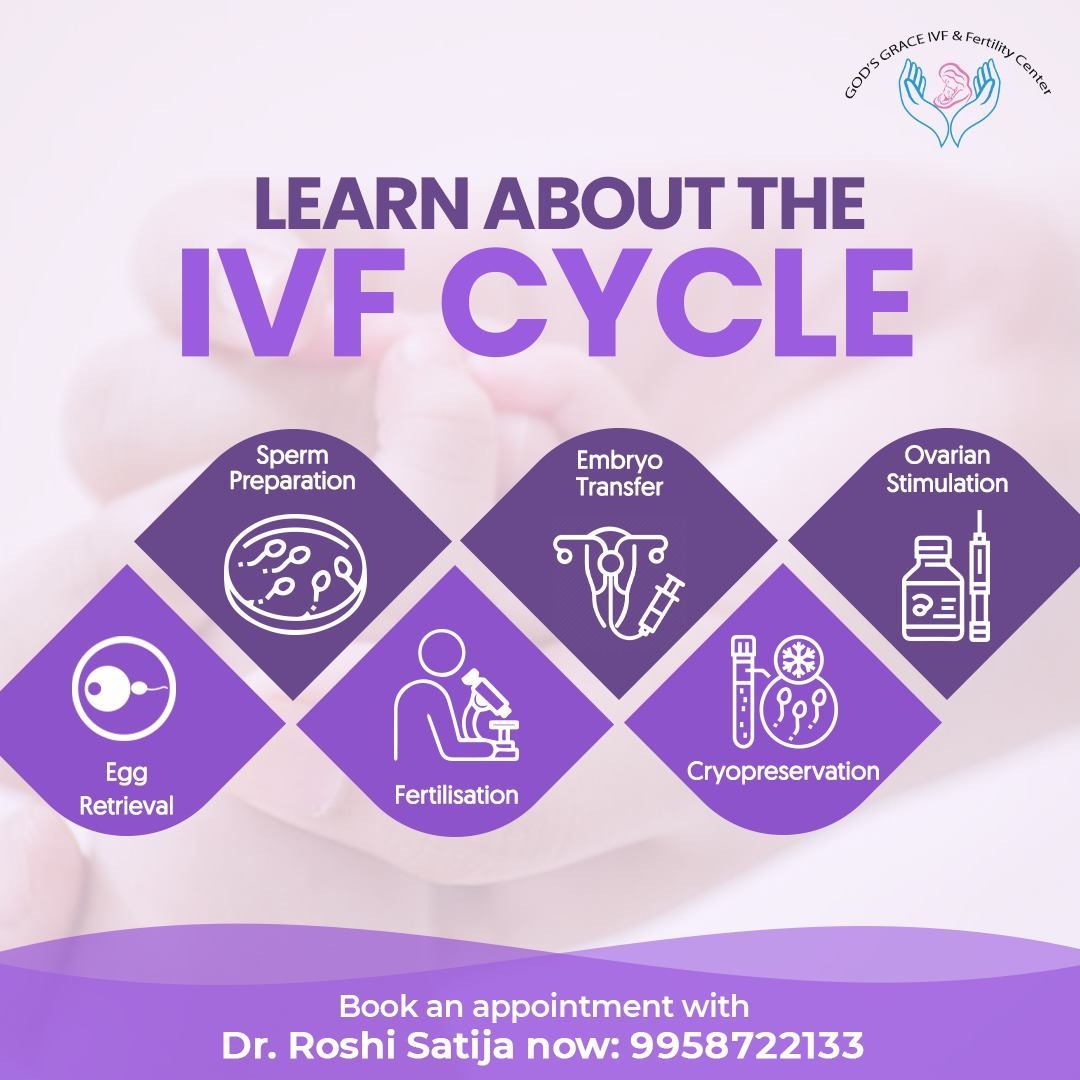
The basic IVF cycle usually includes these stages:
- Ovarian Stimulation – Meds boost your ovaries to produce multiple eggs.
- Egg Retrieval – A quick procedure to collect those eggs.
- Fertilization – Eggs meet sperm in a lab to create embryos.
- Embryo Development – Embryos grow for a few days under close watch.
- Embryo Transfer – One (or more) embryos are placed in your uterus.
- The Two-Week Wait – You wait to see if the embryo implants and you’re pregnant.
Each step has its own timeline, and where you are depends on what you’ve already done. Let’s explore these stages so you can match them to your own experience.
Where Are You in the IVF Timeline?
Every IVF cycle is unique, but most follow a similar rhythm. Here’s how to figure out where you stand based on what’s happening right now.
Stage 1: Ovarian Stimulation (Days 1-14)
This is where it all begins. You’re likely taking hormone shots or pills to get your ovaries working overtime. This phase usually lasts 10-14 days, depending on how your body responds. You’ll visit the clinic for ultrasounds and blood tests to check your egg growth.
- How to Tell You’re Here: Are you giving yourself daily injections? Tracking follicle sizes? Feeling a little bloated or emotional from the meds? If so, you’re in the stimulation zone.
- What’s Happening: Your ovaries are growing multiple follicles (tiny sacs that hold eggs). The goal is to get them to about 18-20 millimeters before retrieval.
- Science Says: According to a 2023 study in Fertility and Sterility, the average number of eggs retrieved increases with longer stimulation (up to a point), but overdoing it can lower egg quality. Balance is key!
Tip: Keep a journal of your symptoms and appointments. It’ll help you spot patterns and feel less lost in the process.
Stage 2: Egg Retrieval (Day 14-16)
Once your follicles are ready, you’ll get a “trigger shot” (usually hCG) to ripen the eggs. About 36 hours later, it’s retrieval day! This minor surgery takes 20-30 minutes under sedation.
- How to Tell You’re Here: Did you just have the trigger shot? Are you prepping for a clinic visit where they’ll use a needle to collect eggs? This is your spot.
- What’s Happening: Doctors use ultrasound to guide a needle through your vaginal wall to suck out the eggs. It sounds intense, but you’ll be asleep!
- Fun Fact: The American Society for Reproductive Medicine (ASRM) says most women produce 8-15 eggs per cycle, though it varies wildly.
Tip: Rest up post-retrieval. Bloating and mild cramping are normal—stock up on cozy socks and a heating pad.
Stage 3: Fertilization and Embryo Growth (Days 16-21)
Now the lab takes over. Your eggs are mixed with sperm (either your partner’s or a donor’s) to create embryos. These little miracles grow for 3-5 days, sometimes up to day 6 or 7 if they’re headed for blastocyst stage.
- How to Tell You’re Here: Are you waiting for a call from the embryologist about how many eggs fertilized? Or how many embryos made it to day 3 or 5? You’re in this waiting game.
- What’s Happening: Embryos are graded for quality. By day 5, the best ones might be blastocysts—ready for transfer or freezing.
- Latest Research: A 2024 study from Human Reproduction found that day 5 blastocysts have a 10-15% higher implantation rate than day 3 embryos. Timing matters!
Interactive Quiz: How many embryos do you think survive to day 5?
- A) All of them
- B) About half
- C) Only 1-2
(Answer: B—about 50% make it, depending on egg and sperm quality!)
Stage 4: Embryo Transfer (Days 21-26)
This is the big moment! A doctor places an embryo (or two) into your uterus using a thin catheter. It’s quick, painless, and doesn’t need anesthesia.
- How to Tell You’re Here: Did you just lie on a table with a full bladder while a doctor used ultrasound to guide the transfer? You’re here!
- What’s Happening: The embryo needs to implant in your uterine lining. Success rates hover around 25-30% per cycle, per ASRM data.
- Unique Insight: Many blogs skip this, but your uterine lining thickness matters. A 2023 study in Reproductive BioMedicine Online suggests a lining of 8-12 mm boosts implantation odds.
Tip: Avoid heavy lifting post-transfer, but don’t stress about “staying still.” Normal activity won’t shake the embryo loose!
Stage 5: The Two-Week Wait (Days 26-40)
The infamous “2WW” is when you wait 10-14 days for a pregnancy test. It’s a mental marathon—hope, anxiety, and Google searches galore.
- How to Tell You’re Here: Are you counting days post-transfer, analyzing every twinge, or resisting the urge to pee on a stick? Welcome to the 2WW!
- What’s Happening: The embryo is (hopefully) implanting and releasing hCG, the pregnancy hormone. A blood test at the clinic will confirm it.
- Science Says: implantation usually happens 6-10 days post-transfer, per a 2024 Journal of Assisted Reproduction report.
Tip: Distract yourself with light hobbies—think puzzles, not powerlifting. Stress won’t ruin your odds, but it’ll make the wait tougher.
How to Track Your Progress Day by Day
Not sure exactly where you are? Here’s a handy day-by-day breakdown of a typical 28-day IVF cycle. Adjust it based on your clinic’s plan!
| Day | What’s Happening | How You Might Feel |
|---|---|---|
| Day 1 | Start stimulation meds | Hopeful, maybe nervous |
| Day 10 | Ultrasound shows follicle growth | Bloated, excited |
| Day 14 | Trigger shot | Relieved it’s almost retrieval |
| Day 16 | Egg retrieval | Groggy, crampy post-procedure |
| Day 21 | Embryo transfer (day 5 blastocyst) | Optimistic, cautious |
| Day 31 | Pregnancy test (10 days post-transfer) | Anxious, fingers crossed |
Pro Tip: Ask your clinic for a personalized calendar. It’s your IVF GPS!
What If You’re Doing a Frozen Embryo Transfer (FET)?
If you’re using frozen embryos, the timeline shifts. You might be asking, “How far along am I in IVF with a frozen cycle?” Here’s the scoop:
- Prep Phase (2-4 weeks): You’ll take estrogen to thicken your lining, then progesterone to mimic a natural cycle. This can start right after retrieval or months later.
- Transfer Day: Similar to a fresh transfer, but no stimulation or retrieval this time.
- 2WW: Same 10-14 day wait for the test.
Unique Insight: Frozen transfers often have slightly higher success rates (up to 35% per cycle, per 2024 ASRM data) because embryos are pre-screened, and your body isn’t recovering from retrieval.
Checklist for FET:
✔️ Track your lining thickness with ultrasounds.
✔️ Confirm progesterone start date with your doc.
❌ Don’t skip meds—timing is everything!
Signs Your IVF Cycle Is on Track
Wondering if things are going well? Look for these green flags at each stage:
- Stimulation: Follicles growing steadily (1-2 mm daily).
- Retrieval: 8+ eggs collected (though quality beats quantity).
- Fertilization: 50%+ of eggs fertilize into embryos.
- Transfer: Smooth procedure, lining looks good.
- 2WW: Mild cramping or spotting (could be implantation!).
Red Flags to Watch:
❌ Slow follicle growth (fewer than 5 by day 10).
❌ Low fertilization rate (less than 30%).
❌ Thin lining (<7 mm) pre-transfer.
If something feels off, chat with your doctor—they’re your co-pilot.
The Emotional Side: How to Cope at Each Stage
IVF isn’t just physical—it’s a mental marathon too. Here’s how to stay sane, stage by stage:
During Stimulation
The hormones can make you feel like a moody teenager. Lean on your partner or a friend who gets it. Try journaling your highs and lows—it’s cheaper than therapy!
Post-Retrieval
You might feel sore and tired. Treat yourself to a Netflix binge and some comfort food (hello, mac and cheese).
The 2WW
This is the toughest part. Avoid symptom-spotting every five minutes—it’ll drive you nuts. Instead, plan a small reward for test day, pregnant or not.
Poll: What’s your go-to distraction during the 2WW?
- A) Binge-watching shows
- B) Baking treats
- C) Talking to friends
(Share your answer in your head—or with a pal!)
What Science Says About IVF Timing and Success
Let’s dig into some fresh data that doesn’t pop up in every IVF blog. A 2024 study in The Lancet tracked 1,000 IVF cycles and found:
- Women under 35 had a 32% live birth rate per cycle.
- Frozen transfers outperformed fresh ones by 5-7% when embryos were genetically tested.
- Day 5 transfers beat day 3 by 12% in implantation success.
Another gem: Timing your transfer with your natural ovulation window (even in a medicated cycle) can bump success rates by 8%, per a 2023 Journal of Fertility Research analysis. Ask your doc if this tweak fits your plan!
Unique Angles You Won’t Find Everywhere
Most IVF guides cover the basics, but here are three points they often miss:
1. The Role of Your Gut Health
Your microbiome might affect implantation. A 2024 Nature Medicine study linked healthy gut bacteria to higher IVF success. How? Good bugs reduce inflammation, which helps embryos stick.
Action Step: Add probiotics (yogurt, kefir) to your diet. Skip this if you’re on antibiotics post-retrieval, though—check with your doc.
2. Micro-Stressors You’re Ignoring
Beyond big stress, little things like poor sleep or caffeine overload can mess with your cycle. A 2023 Sleep Journal study found women sleeping 7-8 hours nightly had 15% better outcomes than those getting under 6.
Fix It: Aim for a consistent bedtime. Swap that third coffee for herbal tea.
3. The Power of Pre-Transfer Rituals
No, not superstition—science! A 2024 Psychology Today report showed women who did a calming ritual (like meditation or a warm bath) pre-transfer had lower cortisol levels and a 10% higher implantation rate.
Try This: Take 10 minutes to breathe deeply or listen to a soothing playlist before your appointment.
Your Next Steps: A Practical Guide
Wherever you are, here’s what to do next:
- Stimulation: Stay hydrated—hormones dehydrate you. Watch for signs of overstimulation (severe pain, rapid weight gain) and call your clinic if they pop up.
- Retrieval: Plan a chill day after. Stock up on electrolyte drinks like Gatorade.
- Transfer: Arrive with a full bladder (it helps the ultrasound). Bring a stress ball to squeeze.
- 2WW: Set daily mini-goals (e.g., “Today I’ll walk 10 minutes”) to keep your mind busy.

Real Stories: Where Others Were in Their IVF Journey
Hearing from others can make this feel less lonely. Meet Sarah, a 32-year-old from Texas:
- “I was on day 12 of stimulation, feeling like a pincushion from all the shots. My ultrasound showed 10 follicles, and I was thrilled—but terrified of retrieval. Knowing it was normal to feel both helped me push through.”
And Jake, a 38-year-old supporting his wife:
- “The 2WW was brutal. She’d cry over a cramp, thinking it meant failure. We made a deal—no early tests. When the call came with a positive, we bawled together.”
Your story’s different, but the emotions? They’re universal.
Wrapping Up: You’re Further Than You Think
So, how far along are you in IVF? Whether you’re jabbing needles, recovering from retrieval, or counting days til the test, you’re moving forward. Each step is a win—proof of your strength and hope. This journey’s not linear, and setbacks happen, but you’re not just a passenger. You’re the driver, steering toward your family.
Take a deep breath. You’ve got this. What’s your next milestone? Celebrate it, big or small—because every day in IVF is a step closer to your goal.


