How Effective Is IVF? A Deep Dive into Success Rates, Real Stories, and What You Need to Know
In vitro fertilization (IVF) has become a household name for people dreaming of starting a family when nature needs a little help. If you’ve ever wondered just how effective IVF really is, you’re not alone—it’s one of the most searched questions about fertility today. Maybe you’re thinking about it for yourself, or maybe you’re just curious about the science behind those tiny test-tube miracles. Either way, this article is here to break it all down for you—success rates, personal stories, the latest research, and even some stuff you won’t find in the usual places. Let’s dive in and explore what makes IVF work (or not), and how it might fit into your life.
What Does “Effective” Mean When It Comes to IVF?
When people ask how effective IVF is, they’re usually wondering one thing: “Will it get me a baby?” That’s the big goal, right? But “effectiveness” in IVF isn’t a one-size-fits-all answer. It’s measured by things like pregnancy rates, live birth rates, and even how many cycles it takes to get there. Doctors and clinics often talk about “success rates,” but those numbers can shift depending on age, health, and a bunch of other factors we’ll unpack.
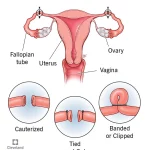
IVF starts with a process where eggs are collected from the ovaries, fertilized with sperm in a lab, and then placed into the uterus. Sounds simple, but there’s a lot going on behind the scenes. The American Society for Reproductive Medicine (ASRM) says that for women under 35, about 40-50% of IVF cycles lead to a live birth. That’s pretty encouraging! But as age goes up, those odds drop—down to about 7-10% for women over 40. So, effectiveness isn’t just about the tech; it’s about you too.
Here’s a quick snapshot of what “effective” might look like:
- ✔️ Pregnancy Rate: The chance of getting pregnant per cycle (think positive test).
- ✔️ Live Birth Rate: The real deal—bringing a baby home.
- ❌ Not a Guarantee: Even with great odds, IVF doesn’t work every time.
Real talk: IVF is a marathon, not a sprint. Most people need more than one try, and that’s totally normal. Let’s dig deeper into what shapes those odds.
Age: The Biggest Player in IVF Success
If there’s one thing that stands out in every study about IVF, it’s age. Your age—or the age of the eggs being used—can make or break the outcome. Why? Because eggs get older, and older eggs are trickier to work with. They’re less likely to fertilize, implant, or grow into a healthy baby.
Check out these numbers from the CDC’s 2022 data:
- Under 35: 51% of egg retrievals result in a live birth.
- 35-37: Drops to about 38%.
- 38-40: Around 24%.
- Over 40: Just 7.6%.
It’s not just about the numbers, though. Younger eggs are usually higher quality—fewer glitches in their DNA. As you hit your late 30s and 40s, the egg supply shrinks, and the ones left might not be as strong. That’s why you’ll hear doctors push for starting IVF sooner if possible.
But here’s a twist: using donor eggs flips the script. If you’re over 40 and use eggs from a younger donor, your success rate jumps back up—sometimes close to 50% per cycle. It’s like borrowing a younger body’s superpower. Pretty cool, right?
What You Can Do About Age
- ✔️ Act Early: If you’re on the fence, talk to a doctor before 35 to get a fertility checkup.
- ✔️ Freeze Eggs: Banking eggs in your 20s or early 30s can lock in better odds for later.
- ❌ Don’t Panic: Age matters, but it’s not the only factor—keep reading!
Beyond Age: What Else Affects IVF Success?
Age might be the headliner, but it’s not the whole show. Your body, lifestyle, and even the clinic you pick play huge roles in whether IVF works. Let’s break it down.
Your Health Matters More Than You Think
Think of your body like a garden—IVF is the seed, but the soil has to be ready. Conditions like polycystic ovary syndrome (PCOS), endometriosis, or low sperm count can throw a wrench in the process. For example, PCOS might mean more eggs but lower quality, while endometriosis can make it harder for an embryo to stick.
Weight plays a part too. Studies—like one from the journal Fertility and Sterility in 2020—show that being significantly underweight or overweight can lower success rates by up to 20%. Why? Hormones get out of whack, and that messes with egg quality and implantation.
Lifestyle Tweaks That Boost Your Odds
Little changes can add up. Research from the ASRM suggests:
- ✔️ Quit Smoking: It cuts success rates by 30%—yikes!
- ✔️ Cut Caffeine: Over 300 mg a day (about 3 coffees) might hurt your chances.
- ❌ Stress Less: Easier said than done, but high stress can mess with hormones.
The Clinic Factor
Not all IVF clinics are created equal. Some have fancy tech or more experienced doctors, which can bump up success rates. The CDC tracks clinic data, and top ones might hit 60% live birth rates for young patients, while others lag at 30%. Picking a good clinic isn’t just about location—it’s about results.
Real Stories: What IVF Success Feels Like
Numbers are great, but stories hit different. Meet Sarah, a 32-year-old teacher from Oregon. After two years of trying naturally, she and her husband turned to IVF. “The first cycle failed, and I was crushed,” she says. “But the second one worked—now we have twins!” Her clinic gave her a 45% shot per cycle, and she beat the odds.
Then there’s Mark, 41, from Texas. His wife was 39, and after three cycles, they still hadn’t had luck. “We switched to donor eggs, and it was like night and day—our son was born last year.” Their story shows how flexibility can turn things around.
These aren’t just feel-good tales—they’re proof that IVF’s effectiveness isn’t just stats. It’s personal, messy, and sometimes magical.
The Numbers Game: Breaking Down Success Rates
Let’s get nerdy for a sec. Success rates are the backbone of IVF talks, but they’re tricky. Clinics love to tout “pregnancy rates,” which sound high—sometimes 60-70% per cycle. But live birth rates? That’s where the rubber meets the road, and those are lower.
Here’s a table to make it clear:
| Age Group | Pregnancy Rate per Cycle | Live Birth Rate per Cycle |
|---|---|---|
| Under 35 | 55-65% | 40-51% |
| 35-37 | 45-55% | 30-38% |
| 38-40 | 35-45% | 20-24% |
| Over 40 | 20-30% | 7-10% |
Why the gap? Miscarriages. About 15-20% of IVF pregnancies don’t make it to birth, especially as age climbs. That’s close to natural conception rates, but it’s still a gut punch when it happens.
Fresh vs. Frozen: Does It Matter?
Another curveball: fresh embryos (used right after egg retrieval) vs. frozen ones (stored for later). A 2023 study in Reproductive BioMedicine Online found frozen embryos might edge out fresh ones by 5-10% in live birth rates. Why? Doctors can prep your body better for a frozen transfer. Something to chew on if you’re planning ahead.
IVF vs. Nature: How Do They Stack Up?
Ever wonder how IVF compares to getting pregnant the old-fashioned way? Naturally, about 70-85% of fertilized eggs don’t implant—way higher than IVF’s failure rate of around 50-70% per cycle. IVF gives you a leg up by picking the best embryos and timing everything just right. It’s like nature with a cheat code.
But here’s the catch: natural conception is free and doesn’t involve needles. IVF costs $15,000-$20,000 a cycle in the U.S., and insurance doesn’t always cover it. So, effectiveness isn’t just about biology—it’s about what you can afford and endure.
The Emotional Rollercoaster: What No One Tells You
IVF isn’t just a physical process—it’s a mind game. The waiting, the hope, the letdowns—it’s a lot. A 2021 study in Human Reproduction found 40% of IVF patients report anxiety or depression during treatment. That’s not in most brochures, but it’s real.
Sarah from earlier? She kept a journal. “Day 10 of waiting for results—I’m a wreck,” she wrote. “But when it worked, it was worth every tear.” Mark said the failures made him question everything, but his son’s first cry erased the doubt. The emotional toll doesn’t show up in success rates, but it shapes the journey.
Coping Tips
- ✔️ Talk It Out: A counselor or support group can lighten the load.
- ✔️ Set Boundaries: Decide how many cycles you’ll try before a break.
- ❌ Don’t Bottle It Up: Ignoring feelings makes it worse.
Mini Quiz: What’s Your IVF IQ?
Let’s take a breather and test your knowledge so far. Answer these quick questions (in your head or on paper—no pressure!):
- What’s the biggest factor in IVF success?
A) Clinic location B) Age C) Diet - True or False: IVF always works on the first try.
- What’s one way to boost your odds?
A) More coffee B) Quitting smoking C) Skipping checkups
(Answers: 1-B, 2-False, 3-B). How’d you do? Stick around—there’s more to learn!
The Science Boost: New Tricks Up IVF’s Sleeve
IVF isn’t stuck in the past—it’s evolving. Here are three cutting-edge ideas shaking things up that you won’t find in every article:
1. AI Picks the Winners
Artificial intelligence is crashing the IVF party. Clinics like those in California are using AI to scan embryos and predict which ones have the best shot. A 2024 trial in Nature Medicine showed AI boosted success rates by 15% for women over 38. It’s like having a super-smart embryo coach.
2. Mitochondrial Magic
Ever heard of mitochondrial replacement? It’s wild—scientists swap out tired mitochondria (the energy packs in cells) in older eggs with fresh ones from a donor. A small 2023 study in Spain saw live birth rates jump from 10% to 25% for women over 40. It’s not mainstream yet, but it’s a game-changer on the horizon.
3. Uterus Prep Hacks
The endometrium (your uterus lining) has to be just right for an embryo to stick. New research from Reproductive Sciences (2025) is testing “personalized transfers”—timing the transfer based on your unique hormone cycles. Early results? Up to 20% better implantation rates. It’s like custom-fitting a cozy bed for your embryo.
These aren’t in every clinic yet, but they show IVF’s future is bright—and more effective than ever.
Money Talks: The Cost of Effectiveness
IVF’s price tag is a biggie. In the U.S., one cycle averages $15,000-$20,000, and most folks need 2-3 tries. That’s $30,000-$60,000 out of pocket if insurance doesn’t chip in. Compare that to the UK, where the NHS might cover it for free if you’re under 43 and meet criteria, or Australia, where Medicare cuts costs to $5,000-$10,000.
Saving Strategies
- ✔️ Shop Around: Clinic prices vary—call a few.
- ✔️ Grants: Groups like BabyQuest offer financial help.
- ❌ Don’t Skimp: Cheaper isn’t always better—check success rates.
A quick calc I did: if your odds are 40% per cycle and you need three tries, you’re looking at a 78% chance of success total (1 – (0.6)^3). Worth it? That’s your call.
What If IVF Doesn’t Work?
Sometimes, IVF doesn’t deliver. It’s tough, but it happens. About 30-50% of couples walk away empty-handed after multiple cycles. What then?
- Donor Options: Eggs, sperm, or embryos from donors can skyrocket success rates.
- Surrogacy: If the uterus is the issue, someone else carrying the baby might work.
- Adoption: Not IVF, but a beautiful Plan B.
Mark’s story with donor eggs is a win, but not everyone’s ready for that leap. And that’s okay—there’s no “right” path, just yours.
Poll Time: What’s Your Take?
Pause for a sec—grab your phone or a sticky note and vote:
- A: IVF is worth it, no matter the cost.
- B: I’d only try if it’s affordable.
- C: I’m not sure it’s for me.
Tally your answer with a friend or in your head. What’s driving your pick? Share in the comments if you’re feeling chatty!
The Hidden Stuff: Three Things You Didn’t Know
Most articles stop at age and success rates, but IVF’s got layers. Here are three under-the-radar points that deserve more airtime:
1. Sperm’s Secret Role
Eggs get all the hype, but sperm quality is half the equation. A 2022 study in Andrology found that DNA damage in sperm cuts success rates by 25%—even with young eggs. Clinics can test for this now, but it’s not routine. Ask about it if you’re hitting roadblocks.
2. The Freeze Factor
Freezing eggs or embryos isn’t just for later—it might help now. A 2024 paper in Fertility and Sterility showed that women who froze eggs early in treatment (say, at 33) and used them later had 10% higher success rates than those who went straight to fresh cycles. It’s like hitting pause to get a better shot.
3. Your Gut’s in the Game
Bet you didn’t see this coming—your gut health might sway IVF. A small 2023 study from UCLA linked a balanced microbiome (think probiotics, less junk food) to better implantation rates. It’s early days, but eating yogurt might just be your new IVF hack.
These nuggets show there’s more to IVF than meets the eye. Digging into them could tip the scales.
Steps to Your Best Shot at IVF
Ready to give IVF a go? Here’s a game plan to max out your chances, broken into simple steps:
- Get Checked: See a fertility doc for tests—egg count, sperm health, the works.
- Pick a Clinic: Look at CDC stats, not just Yelp reviews.
- Prep Your Body: Eat well, sleep more, ditch the cigs—give your “garden” a boost.
- Ask Questions: Will you use fresh or frozen? Any AI or extras on the table?
- Plan the Cash: Save up or hunt for grants—don’t let money sneak up on you.
Each step stacks the deck a little more in your favor. No guarantees, but you’re in the driver’s seat.
Wrapping It Up: Is IVF Effective for You?
So, how effective is IVF? It’s a powerhouse—50% odds for the young crowd, a lifeline for older folks with donor eggs, and a tech marvel that’s only getting better. But it’s not magic. It’s a mix of science, luck, and grit, shaped by your age, health, and choices. For Sarah, it was twins after two tries. For Mark, it was a donor egg win. For you? It’s your story to write.
The real kicker: IVF’s effectiveness isn’t just about babies—it’s about hope. Every cycle’s a shot at something huge, and even the misses teach you something. Whether it’s worth it depends on your wallet, your heart, and how far you’re willing to go. What do you think—could IVF be your game-changer?
Your Turn: Checklist Time
Before you bounce, grab this quick checklist to kick things off:
- ✔️ Book a fertility consult.
- ✔️ Research two clinics near you.
- ✔️ Jot down one lifestyle tweak to try this week.
Got questions? Drop them below—I’m here to chat! Let’s keep this convo going.