How Does the IVF Timeline Work? Your Step-by-Step Guide to In Vitro Fertilization
Starting a family can feel like a big adventure, but for some, it’s not as simple as it seems. If you’ve been trying to have a baby and things aren’t clicking, you might have heard about in vitro fertilization, or IVF. It’s a process that’s helped millions of people become parents, and while it might sound a little sci-fi—mixing eggs and sperm in a lab—it’s actually a well-traveled road for many. So, how does it all work? How long does it take? Let’s walk through the IVF timeline together, step by step, with all the details you need to feel ready and in the know.
IVF isn’t a one-day deal. It’s a journey that unfolds over weeks, sometimes months, depending on your unique situation. From the first doctor’s visit to that hopeful pregnancy test, every stage has a purpose. Whether you’re just curious or seriously considering it, this guide breaks it all down into bite-sized pieces. Plus, we’ll dig into some fresh angles—like how your lifestyle can tweak the process, what new research says about success rates, and even a peek at what happens behind the scenes in the lab. Ready? Let’s dive in.
What Is IVF, Anyway?
IVF stands for in vitro fertilization, which is a fancy way of saying “fertilization in glass.” Basically, it’s when doctors take eggs from a woman’s ovaries, mix them with sperm in a lab, and then place the resulting embryo (or embryos) back into the uterus to grow into a baby. It’s part of a bigger category called assisted reproductive technology (ART), and it’s been around since 1978, when the first IVF baby, Louise Brown, was born in England.
Think of it like giving nature a little nudge. If sperm and eggs can’t meet up on their own—maybe because of blocked tubes, low sperm count, or other hurdles—IVF steps in to make it happen. The timeline can vary, but a full cycle usually takes about 4 to 6 weeks from start to finish. That’s just the core process, though—prep work and follow-ups can stretch it out a bit longer.
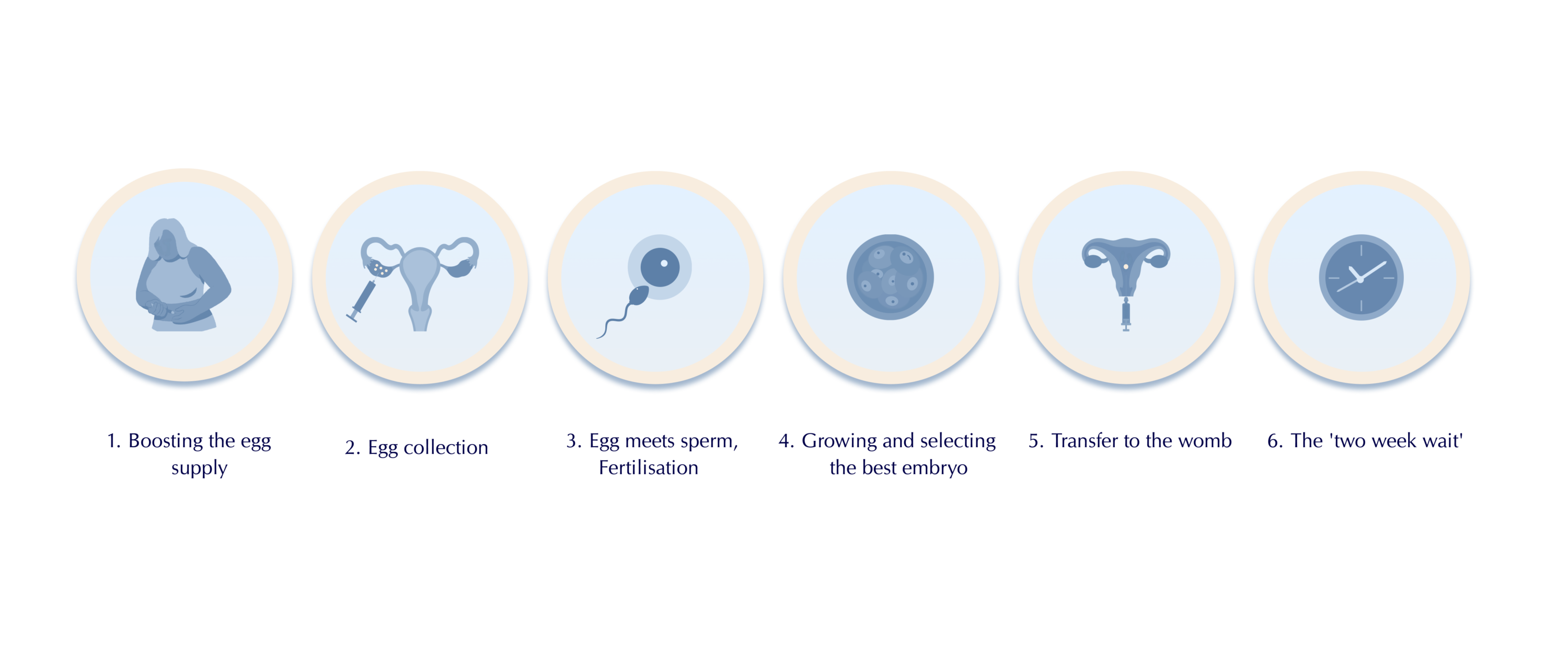
The IVF Timeline: Breaking It Down Step by Step
Every IVF journey is personal, but the process follows a pretty standard path. Here’s how it typically goes, with all the details you might be wondering about—like how long each part takes, what it feels like, and what’s happening in your body.
Step 1: Getting Ready (1-2 Months Before the Cycle)
Before anything starts, you’ll need a game plan. This prep phase can take a month or two, depending on your doctor and your body’s rhythm. It’s all about making sure you’re in the best possible shape for what’s ahead.
First, you’ll meet with a fertility specialist. They’ll ask about your health history, run some tests—like blood work to check hormone levels or an ultrasound to peek at your ovaries—and maybe even test your partner’s sperm if that’s part of the picture. This is also when you might get a heads-up about lifestyle tweaks, like cutting back on caffeine or stress, which studies show can boost your odds.
Sometimes, doctors prescribe birth control pills for a few weeks. Sounds weird, right? But it’s to sync your cycle and calm your ovaries down so they’re ready to roll when the real action starts. Think of it like hitting the reset button.
- How long? 4-8 weeks, depending on testing and your menstrual cycle.
- What’s the goal? To map out your treatment and get your body primed.
Quick Tip: Start a journal during this phase. Jot down questions for your doctor or how you’re feeling—it can help you stay grounded.
Step 2: Ovarian Stimulation (10-14 Days)
Now the fun begins! This step is all about getting your ovaries to produce more eggs than they usually do (which is just one per month in a natural cycle). You’ll take fertility drugs—usually shots you give yourself in your belly or thigh—to kick things into high gear.
These meds, like follicle-stimulating hormone (FSH), tell your ovaries, “Hey, let’s make a bunch of eggs!” Over 10 to 14 days, those eggs grow inside tiny sacs called follicles. Your doctor will check in with ultrasounds and blood tests every few days to see how things are progressing. It’s a bit like tending a garden—you’re watching those little buds sprout.
- How long? About 2 weeks.
- What’s it feelAUC like? You might feel bloated or moody from the hormones—totally normal.
- Science bit: A 2023 study from the American Society for Reproductive Medicine found that tweaking these meds based on your age and hormone levels can up your egg count by 15%.
Checklist for Success:
✔️ Stick to your shot schedule—set phone reminders!
✔️ Eat well—protein and healthy fats can support egg quality.
❌ Skip the gym’s heavy workouts; light walks are better now.

Step 3: The Trigger Shot (36 Hours Before Retrieval)
When your follicles are big enough (usually 18-20 millimeters), it’s time for the trigger shot. This is a dose of human chorionic gonadotropin (hCG) or another hormone that says, “Eggs, get ready to launch!” Timing here is clutch—about 36 hours later, you’ll head in for egg retrieval. Too early or too late, and the eggs might not be ripe.
- How long? A quick injection, then a 36-hour wait.
- What’s happening? Your eggs finish maturing and loosen up for pickup.
Pro Tip: Have a chill day planned after the shot. Stress can mess with your vibe, so binge a show or read something light.
Step 4: Egg Retrieval (30-60 Minutes)
This is the big moment! You’ll go to the clinic, get some light sedation (you’ll be awake but super relaxed), and the doctor will use an ultrasound-guided needle to scoop those eggs out of your ovaries. It’s quick—about 30 minutes—and you’ll rest for an hour or so after.
Meanwhile, if your partner’s providing sperm, they’ll do their part that day too. The lab team takes over from here, pairing eggs with sperm to start the magic.
- How long? Half a day, including recovery.
- What’s it like? A little cramping afterward, but sedation keeps it comfy.
- Fun fact: On average, doctors retrieve 8-15 eggs, though it varies.
Post-Retrieval Plan:
✔️ Rest up—take the day off if you can.
✔️ Sip water; hydration helps recovery.
❌ Don’t freak out over mild spotting—it’s common.
Step 5: Fertilization and Embryo Growth (3-6 Days)
In the lab, your eggs meet the sperm. Sometimes it’s old-school—sperm and eggs mingle in a dish—or they might use intracytoplasmic sperm injection (ICSI), where one sperm is injected right into an egg. Either way, the goal is embryos.
For the next 3 to 6 days, those embryos grow under a microscope. The embryologist watches them like a hawk, picking the strongest ones. By day 5 or 6, they’re often at the blastocyst stage—ready to roll.
- How long? 3-6 days.
- What’s new? Some clinics now use time-lapse imaging to track embryo growth without disturbing them—cool, right?
Interactive Moment: How Many Embryos Survive?
Take a guess! On average, what percentage of fertilized eggs make it to the blastocyst stage?
- A) 20-30%
- B) 40-50%
- C) 70-80%
(Answer’s at the end—keep reading!)
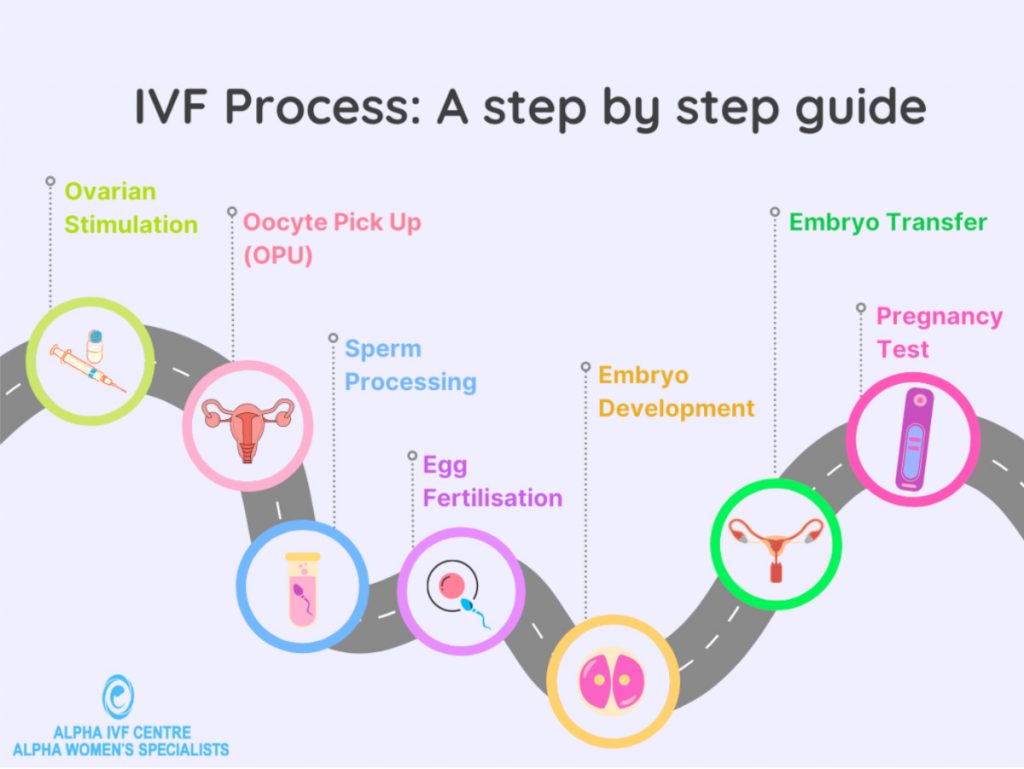
Step 6: Embryo Transfer (15-20 Minutes)
Time to put those embryos to work! You’ll head back to the clinic, no sedation needed this time. The doctor slides a thin catheter through your cervix and places one (or sometimes two) embryos into your uterus. It’s quick and feels like a Pap smear.
After, you’ll lie down for 20-30 minutes, then head home. Some embryos might get frozen for later if you’ve got extras—think of it as a backup plan.
- How long? A short visit, but the wait afterward is key.
- What’s it feel like? Mild cramping, maybe some nerves.
Aftercare Tips:
✔️ Take it easy for a day or two—think couch and cozy socks.
✔️ Stay positive—stress won’t help implantation.
❌ Don’t test too early; wait for the official check.
Step 7: The Two-Week Wait (10-14 Days)
Now, you wait. About 10-14 days after the transfer, you’ll take a blood test to see if you’re pregnant. This “two-week wait” can feel endless—your embryo is (hopefully) snuggling into your uterine lining, but you won’t know yet.
- How long? 2 weeks that test your patience.
- What’s happening? Hormones like progesterone (via pills or shots) support your uterus.
Coping Ideas:
✔️ Distract yourself—craft, cook, or call a friend.
✔️ Lean on your support crew—talk it out.
❌ Avoid Googling every twinge; it’ll drive you nuts.
Step 8: Pregnancy Test and Beyond (Day 14+)
The moment of truth! A blood test checks for hCG, the pregnancy hormone. If it’s positive, congrats—you’re on your way! You’ll likely have an ultrasound in a few weeks to confirm everything’s on track. If it’s negative, your doctor will talk next steps, like using frozen embryos or tweaking the plan.
- How long? A quick test, but the journey’s just beginning—or shifting.
- Success stats: In 2021, the CDC reported a 45% live birth rate for women under 35 per egg retrieval cycle. It drops with age, but every case is unique.
How Long Does IVF Really Take? A Full Picture
Adding it all up, a single IVF cycle—from the first fertility shot to the pregnancy test—takes about 4-6 weeks. But factor in the prep (1-2 months) and any hiccups (like canceled cycles or extra testing), and you’re looking at 2-4 months total for one go. If you need multiple cycles or frozen embryo transfers, it could stretch to a year or more.
Here’s a handy timeline table:
| Stage | Duration | What’s Happening |
|---|---|---|
| Prep | 1-2 months | Testing, planning, maybe birth control |
| Stimulation | 10-14 days | Eggs grow with hormone shots |
| Trigger + Retrieval | 2 days | Eggs mature and get collected |
| Embryo Growth | 3-6 days | Eggs fertilize and develop |
| Transfer | 1 day | Embryo placed in uterus |
| Two-Week Wait | 10-14 days | Waiting for pregnancy test |
Reality Check: About 5% of infertile couples try IVF, and over 8 million babies have been born this way since 1978, per Cleveland Clinic data. You’re not alone on this road.
What Affects the IVF Timeline?
Not every IVF journey follows the same clock. Here’s what can speed it up or slow it down—and some stuff the top articles don’t always dig into.
Your Age and Health
Age is a biggie. If you’re under 35, your eggs are usually top-notch, and success rates hover around 40-50% per cycle. Over 40? It drops to under 10%, says Yale Medicine. Health stuff—like PCOS or endometriosis—can mean extra steps, like surgery or longer stimulation.
Fresh vs. Frozen Embryos
Some folks do a “fresh” transfer right after retrieval. Others freeze embryos and transfer later—maybe to rest their body or test embryos for genetic issues. Frozen transfers add a month or two but can boost success rates by 5-10%, per a 2022 study.
Lifestyle Factors (The Unsung Hero)
Here’s a fresh take: what you eat, drink, and do matters more than you’d think. A 2024 report from the University of Toronto found that women who ate a Mediterranean diet (think fish, veggies, olive oil) during IVF had 20% more viable embryos. Stress busters like yoga? They cut cortisol levels, which might help implantation.
Try This:
- Swap coffee for herbal tea—caffeine can mess with egg quality.
- Take a 10-minute walk daily—movement without overdoing it.
Behind the Scenes: What Happens in the Lab?
Ever wonder what’s going on while you’re waiting? The lab is where the real magic happens, and it’s not talked about enough. After retrievalcony, eggs get a spa day—sort of. They’re cleaned, checked for maturity, and paired with sperm. If ICSI’s in play, a tiny needle delivers the sperm right into the egg—precision at its finest.
Embryos grow in incubators mimicking your body’s temp and pH. New tech, like AI-driven embryo selection, is starting to predict which ones have the best shot. A 2023 trial showed AI bumped success rates by 12% in some clinics. It’s like having a super-smart babysitter for your future kid.
Real Talk: What’s It Like Emotionally?
The timeline’s not just physical—it’s an emotional rollercoaster. One day you’re hopeful; the next, you’re googling “why didn’t it work?” A 2024 survey of 500 IVF patients found 70% felt overwhelmed during the two-week wait. But here’s the flip side: 85% said support—friends, family, or online groups—made it bearable.
Interactive Poll:
What’s your go-to stress buster during waiting periods?
- A) Netflix marathon
- B) Talking it out
- C) Something active (walk, yoga)
(Share your pick in your head—or with a friend!)
New Research: What’s Changing the Game?
IVF’s always evolving. Here are three cutting-edge updates you won’t find in every article:
- Mitochondrial Boosts: Older eggs often lack energy. A 2023 study tested adding coenzyme Q10 (CoQ10) to the mix, finding a 15% jump in embryo quality for women over 38. Ask your doc about supplements!
- Mini-IVF: Using fewer drugs for a gentler cycle is gaining traction. It’s cheaper and less intense, with success rates nearing 30% for younger patients, per a 2024 review.
- Endometrial Receptivity Tests: These check if your uterus is ready for an embryo. A 2022 trial showed a 10% higher implantation rate when transfers matched the “receptive window.”
Unique Tips for Your IVF Journey
Most guides stick to the basics, but here’s some extra wisdom to make your timeline smoother:
- Track Your Meds Like a Pro: Use a color-coded calendar—blue for shots, red for appointments. It’s less chaotic than a phone app.
- Freeze Sperm Early: If your partner’s schedule’s tricky, banking sperm ahead avoids last-minute stress.
- Mock Transfer: Some clinics do a practice run before the real transfer. It’s not standard, but it can spot issues (like a tricky cervix) early.
Case Study: Sarah, 34, from California, did IVF in 2024. Her clinic suggested a mock transfer after a failed cycle. Round two? She’s now 6 months pregnant. Small tweaks can make a big difference.
What If It Doesn’t Work the First Time?
Not every cycle ends with a plus sign. About 50% of first attempts don’t stick, but that’s not the end. Frozen embryos give you another shot without starting over. And doctors can adjust—maybe more meds, a different protocol, or genetic testing. A 2023 stat: women who tried 3 cycles had a 65% chance of success overall.
Next Steps:
✔️ Ask about embryo quality—what went wrong?
✔️ Consider a break—your body might need it.
❌ Don’t blame yourself; biology’s tricky.


