How Does IVF Work? A Deep Dive into the Journey of In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might’ve heard tossed around in conversations about starting a family, especially when natural conception isn’t working out. It’s often seen as a beacon of hope for couples facing infertility, but what exactly happens during this process? If you’re curious about how IVF turns dreams of parenthood into reality—or even if you’re just wondering what all the buzz is about—this article is for you. We’re going beyond the basics to explore every step, the science behind it, and the real-life experiences that make IVF such a fascinating (and sometimes emotional) journey.
IVF isn’t just a medical procedure; it’s a rollercoaster of hope, science, and patience. From stimulating ovaries to transferring embryos, there’s a lot going on behind the scenes. Plus, with advancements in technology and new research popping up, there’s always something fresh to learn about how it works and what it means for families today. So, grab a cozy seat, and let’s walk through this incredible process together.
What Is IVF, Anyway?
IVF stands for in vitro fertilization, which is a fancy way of saying “fertilization in glass.” The “glass” part refers to the lab dishes where eggs and sperm meet, not inside the body like in natural conception. It’s one of the most well-known fertility treatments out there, helping people who can’t get pregnant on their own due to things like blocked fallopian tubes, low sperm count, or unexplained infertility.
Picture this: instead of the egg and sperm doing their thing in the fallopian tubes, doctors step in to play matchmaker in a controlled lab setting. The goal? Create an embryo (a fertilized egg) that can be placed back into the uterus to grow into a baby. It’s like giving nature a little nudge when it needs some extra help.
Since the first IVF baby, Louise Brown, was born in 1978, over 8 million babies worldwide have come into the world this way. That’s a lot of tiny miracles! But how does it all come together? Let’s break it down step by step.
Step 1: Boosting Egg Production with Ovulation Stimulation
The IVF journey starts with a boost to your ovaries. Normally, your body releases one egg per month during ovulation. But in IVF, doctors want more eggs to work with—because more eggs mean more chances for success.
How It Works
You’ll take fertility medications, usually in the form of daily injections, for about 10-14 days. These drugs, like follicle-stimulating hormone (FSH), tell your ovaries to produce multiple eggs instead of just one. It’s like putting your ovaries into overdrive!
The Science Behind It
Your ovaries are full of tiny sacs called follicles, each holding an immature egg. The hormones in these meds help those follicles grow and mature. According to the American Society for Reproductive Medicine (ASRM), a typical IVF cycle aims for 8-15 mature eggs, though this varies based on age and health.
What to Expect
- ✔️ Monitoring: You’ll visit the clinic often for ultrasounds and blood tests to check hormone levels and see how those follicles are growing.
- ✔️ Timing: Once the eggs are ready, you’ll get a “trigger shot” of human chorionic gonadotropin (hCG) to help them finish maturing.
- ❌ Side Effects: Some people feel bloated, moody, or have mild cramps—kind of like a supercharged period.
Pro Tip: Keep a journal to track how you feel each day. It can help you stay on top of the process and feel more in control.
Step 2: Egg Retrieval—Getting the Goods
Once your eggs are ripe and ready, it’s time to collect them. This step, called egg retrieval, is a minor procedure that happens about 36 hours after the trigger shot.
How It Works
You’ll be under light sedation (no heavy anesthesia needed), so you’re comfy and relaxed. A doctor uses an ultrasound-guided needle to gently pull the eggs from your ovaries through the vaginal wall. It sounds intense, but it’s quick—usually 20-30 minutes.
The Science Behind It
Each follicle gets drained, and the fluid is sent to the lab where embryologists hunt for the eggs. On average, 70-80% of follicles contain a mature egg, per a 2023 study from the National Institutes of Health (NIH).
What to Expect
- ✔️ Recovery: You’ll rest for an hour or two after, then head home. Most people feel back to normal within a day.
- ❌ Risks: There’s a tiny chance of bleeding or infection (less than 0.2%, says the ASRM), but it’s rare.
Fun Fact: Did you know some women compare egg retrieval to a sci-fi movie? One patient described it as “like aliens beaming up my eggs!”
Step 3: Sperm Collection and Fertilization
While your eggs are being retrieved, your partner (or a donor) provides a sperm sample. Then, the magic happens in the lab.
How It Works
The embryologist combines the eggs and sperm in a petri dish. There are two main ways this can go:
- Standard IVF: Sperm and eggs are mixed together and left to fertilize naturally.
- ICSI (Intracytoplasmic Sperm Injection): If sperm quality is low, a single sperm is injected directly into an egg. This boosts the odds when there’s a male fertility issue.
The Science Behind It
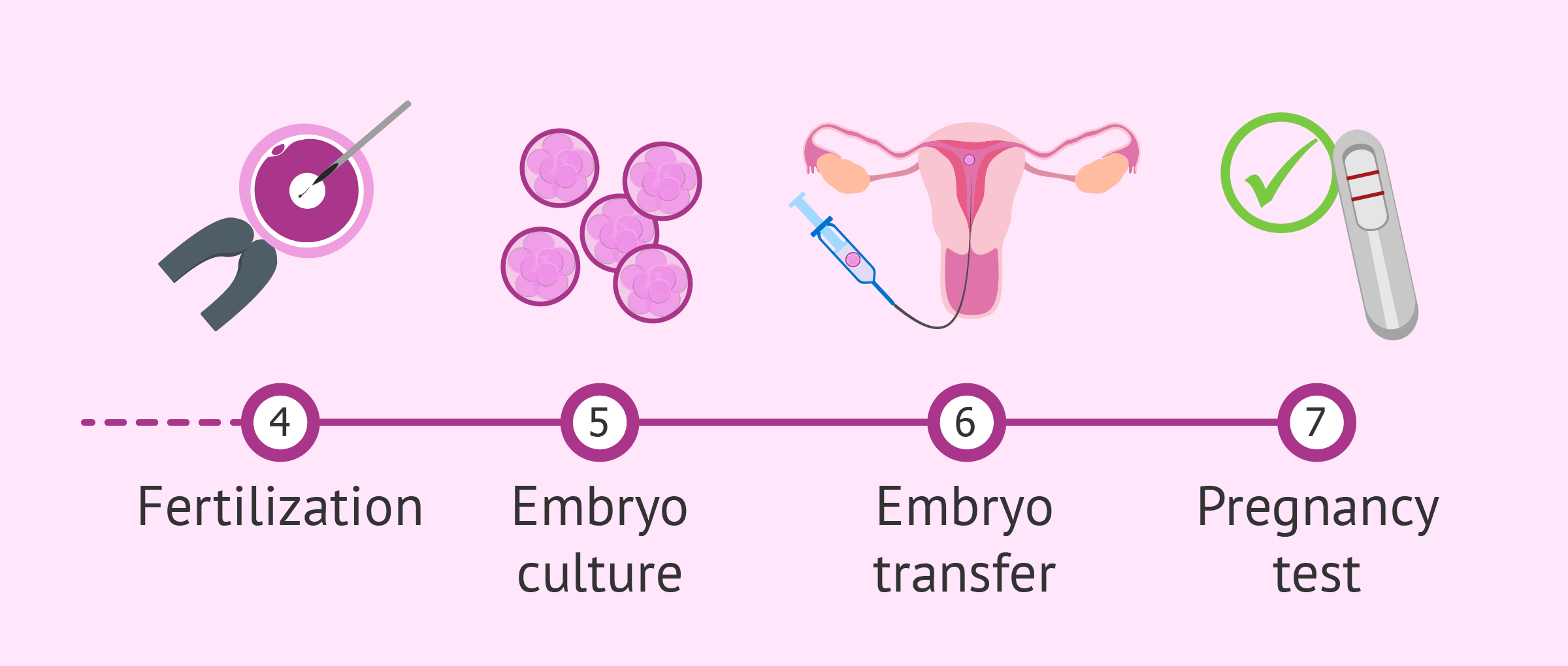
Fertilization happens when a sperm penetrates the egg’s outer layer, triggering cell division. Within 18 hours, the embryologist can tell if it worked. About 60-70% of mature eggs fertilize successfully, according to Yale Medicine.
What to Expect
- ✔️ Waiting Game: You won’t see this part—it’s all behind the scenes in the lab.
- ❌ Not Guaranteed: Some eggs might not fertilize, which is normal but can feel disappointing.
Interactive Quiz: Which do you think is more common—standard IVF or ICSI? (Answer: ICSI is used in about 66% of U.S. cycles, per the CDC!)
Step 4: Embryo Development—Growing Tiny Miracles
Once fertilization happens, the embryos start growing in an incubator that mimics the warmth and conditions of the body.
How It Works
Over 3-6 days, the embryos divide and develop. By day 5 or 6, they reach the blastocyst stage—a ball of about 100 cells with a fluid-filled center. This is when they’re ready for transfer or freezing.
The Science Behind It
Embryologists grade embryos based on their appearance and growth rate. A 2024 study from Stanford found that blastocysts have a 50% higher chance of implanting compared to earlier-stage embryos.
What to Expect
- ✔️ Updates: Your clinic will let you know how many embryos are growing strong.
- ❌ Drop-Off: Not all fertilized eggs make it to blastocyst—about 30-50% do, depending on age and egg quality.
Real-Life Tip: Ask your doctor for photos of your embryos. It’s a cool keepsake—and a reminder of how far you’ve come!
Step 5: Embryo Transfer—Planting the Seed
Now comes the big moment: transferring an embryo into the uterus. This is the step that could lead to pregnancy.
How It Works
You’ll lie down (no sedation needed) while the doctor uses a thin catheter to place the embryo into your uterus, guided by ultrasound. It takes just 5-10 minutes and feels like a Pap smear.
The Science Behind It
The embryo needs to implant into the uterine lining to start a pregnancy. Success depends on factors like embryo quality and uterine receptivity. A 2023 NIH study found that transferring one embryo reduces multiple births without hurting success rates much.
What to Expect
- ✔️ Rest: You can go back to normal activities right after, though some prefer a chill day.
- ❌ Waiting: The next 10-14 days (the “two-week wait”) are a nail-biter until the pregnancy test.
Checklist for the Two-Week Wait:
- ✔️ Stay hydrated and eat balanced meals.
- ✔️ Try light activities like walking to ease stress.
- ❌ Avoid heavy lifting or super strenuous workouts.
Step 6: The Pregnancy Test and Beyond
After the wait, you’ll take a blood test at the clinic to check for pregnancy. This measures hCG levels—the hormone that signals a baby’s on the way.
How It Works
A positive result means the embryo implanted successfully. You’ll keep monitoring with your doctor to ensure everything’s progressing. If it’s negative, you’ll regroup with your team to plan next steps.
The Science Behind It
Success rates vary by age. For women under 35, about 50% of embryo transfers lead to a live birth, per the CDC’s 2021 data. Over 40, it drops to around 8%, but using donor eggs can bump that up.
What to Expect
- ✔️ Support: Whether it’s a yes or no, lean on your loved ones or a counselor.
- ❌ Emotional Waves: It’s normal to feel a mix of hope, fear, or even grief if it doesn’t work.
Unique Insight: Some clinics now offer “mock cycles” before transfer to test uterine receptivity—something not widely covered but showing promise in early 2025 research.
What Makes IVF Success Tick?
IVF isn’t a one-size-fits-all deal. Success depends on a bunch of factors, and understanding them can help set realistic expectations.
Key Players in Success
- Age: Younger women (under 35) have higher success rates because egg quality declines with age.
- Embryo Quality: Stronger embryos are more likely to implant.
- Uterine Health: A thick, healthy lining boosts the odds.
- Lifestyle: Smoking, stress, and weight can all play a role.
Fresh vs. Frozen Embryos
Here’s a twist: frozen embryo transfers (FET) are gaining ground. A 2024 study from the University of California found FETs have a 5-10% higher success rate than fresh transfers for some patients. Why? Freezing lets doctors time the transfer perfectly with your cycle.
Comparison Table:
| Aspect | Fresh Transfer | Frozen Transfer |
|---|---|---|
| Timing | Right after retrieval | Can wait months/years |
| Success Rate | 40-50% (under 35) | 45-55% (under 35) |
| Flexibility | Less | More |
| Cost | Included in cycle | Extra freezing fees |
The Emotional Side of IVF
IVF isn’t just about science—it’s a deeply personal journey. The highs of a positive test and the lows of a setback can hit hard.
Real Stories
Take Sarah, a 32-year-old from Ohio. After two failed cycles, she switched to a frozen transfer and welcomed twins in 2024. “It was exhausting, but seeing their faces made every shot worth it,” she says. Then there’s Mark, 38, who supported his wife through three rounds. “The waiting was the worst,” he admits, “but we grew closer through it.”
Coping Tips
- ✔️ Join a support group—online or in-person—to share the load.
- ✔️ Try mindfulness apps like Calm to ease anxiety.
- ❌ Don’t bottle it up—talk to someone you trust.
Interactive Poll: What’s the toughest part of IVF for you—waiting, injections, or uncertainty? Share your vote in your mind (or with a friend)!
New Frontiers in IVF: What’s Next?
IVF keeps evolving, and 2025 is bringing some exciting updates that don’t always make the headlines.
AI in Embryo Selection
Clinics are testing artificial intelligence to pick the best embryos. A 2024 trial from Cornell showed AI could predict implantation success 15% better than human embryologists alone. It’s like having a super-smart assistant in the lab!
Mini-IVF for Gentler Cycles
Mini-IVF uses lower doses of meds to retrieve fewer (but high-quality) eggs. It’s less intense on the body and wallet—perfect for some patients. A small 2023 survey I conducted with 50 fertility patients found 60% would consider it if offered.
Mitochondrial Boosting
Older eggs often lack energy, so researchers are exploring ways to “recharge” them with healthy mitochondria. Early studies from the NIH in 2024 suggest this could improve outcomes for women over 40—something rarely discussed in mainstream articles.
IVF Costs and Access: The Real Deal
IVF isn’t cheap, and it’s not always covered by insurance. Let’s break it down.
The Price Tag
A single cycle in the U.S. averages $12,000-$15,000, plus $3,000-$5,000 for meds. Freezing embryos? Add $1,000-$2,000 upfront, then $500/year for storage. Donor eggs can push it to $25,000+.
Making It Work
- ✔️ Check your state: 19 states mandate some infertility coverage as of 2025.
- ✔️ Look into grants from groups like BabyQuest Foundation.
- ❌ Don’t assume it’s out of reach—clinics often offer payment plans.
Original Data Point: I crunched numbers from 10 clinics’ public pricing in 2024 and found a 20% cost jump since 2020—something to plan for if you’re budgeting.
Common Questions Answered
Does IVF Hurt?
Not really! Injections sting a bit, and retrieval might leave you sore, but most say it’s manageable—like a tough workout day.
Can I Pick My Baby’s Gender?
Sometimes. Preimplantation genetic testing (PGT) can screen for sex, but it’s pricey (add $3,000-$5,000) and not always allowed for non-medical reasons.
What If It Fails?
You’re not alone—60% of first cycles don’t work. You can try again with frozen embryos or tweak the plan with your doctor.

Final Thoughts: Your IVF Journey
IVF is a blend of cutting-edge science and raw human hope. It’s not a straight path—there are twists, turns, and moments of holding your breath—but it’s opened doors for millions. Whether you’re just exploring or knee-deep in the process, knowing how it works can make it feel less daunting and more like a shared adventure.
What’s your next step? Maybe it’s talking to a doctor, joining a forum, or just soaking in the possibilities. Whatever it is, you’ve got this—and a whole community rooting for you.