Does IVF Increase Your Risk of Cancer?
In vitro fertilization (IVF) has been a game-changer for millions of people dreaming of starting a family. It’s a beacon of hope for those facing infertility, turning what once felt impossible into a real possibility. But with all the incredible stories of success, there’s a question that keeps popping up: Could IVF come with a hidden cost—like an increased risk of cancer? If you’re considering IVF or just curious about how it works, you’ve probably wondered about this too. The idea of pumping your body with hormones to make a baby can feel a little daunting, right? So, let’s dive in and unpack this topic together—looking at the science, the myths, and what it all means for you.
What Is IVF, Anyway?
IVF is a process where doctors help create a baby outside the body. They take an egg from a woman’s ovaries, mix it with sperm in a lab, and then place the resulting embryo back into the uterus to grow. To get those eggs ready, women take hormone medications—like follicle-stimulating hormone (FSH) or gonadotropins—to boost egg production. It’s a bit like giving your ovaries a pep talk to work overtime.
Now, here’s where the cancer question comes in. Those hormones increase estrogen and progesterone levels in your body, and some cancers—like breast or ovarian cancer—are known to be sensitive to hormones. Naturally, people wonder: Could this extra hormone boost tip the scales toward cancer? It’s a fair concern, and one that researchers have been digging into for years.
The Big Question: Does IVF Cause Cancer?
When you type “Does IVF increase cancer risk?” into Google, you’ll find a mix of answers—some reassuring, some alarming. The truth? It’s not a simple yes or no. Studies have been piling up since IVF became common in the 1980s, and the good news is that the overall picture looks pretty positive. Let’s break it down by the types of cancer people worry about most: breast, ovarian, and endometrial (uterine) cancer.
Breast Cancer and IVF: What’s the Connection?
Breast cancer is one of the most common cancers women face, so it’s no surprise it’s a big focus when we talk about IVF. The hormones used in IVF, especially estrogen, can make some breast cancers grow faster if they’re already there. But does IVF cause breast cancer to start?
A massive study from the Netherlands, published in 2016, followed over 19,000 women who had IVF and compared them to 6,000 women who didn’t. After 21 years, they found no significant increase in breast cancer risk among the IVF group. Another study from Sweden, looking at over 24,000 women who gave birth via IVF, actually found a lower risk of breast cancer—24% less than women who conceived naturally. Why? It might be because women who successfully have babies through IVF often breastfeed, which is known to lower breast cancer risk.
But here’s a twist that doesn’t get talked about enough: age matters. Women starting IVF over 30 might face a slightly higher risk, according to a smaller Australian study. It’s not a huge jump, but it suggests timing could play a role—something we’ll explore more later.
Ovarian Cancer: A Deeper Look
Ovarian cancer is rarer but scarier because it’s often caught late. Since IVF stimulates the ovaries like crazy, people wonder if that could lead to trouble down the road. The “incessant ovulation” theory says that the more your ovaries ovulate, the higher your risk of cancer—because each ovulation causes tiny damage that might go haywire.
Here’s the reassuring part: A 2020 study from the Netherlands followed over 40,000 women for 24 years and found no link between IVF and invasive ovarian cancer. Even women who had multiple IVF cycles didn’t show a higher risk. However, there was a catch—they did see a slight uptick in borderline ovarian tumors, which are less dangerous and often curable. The risk went from 0.2% to 0.3% for women over 55—not a big leap, but worth noting.
What’s really interesting? Women who never had kids (nulliparous) had a higher ovarian cancer risk, whether they did IVF or not. So, it might be infertility itself—not the IVF—that’s the real factor here.
Endometrial Cancer: Hormones and the Uterus
Endometrial cancer affects the lining of the uterus, and it’s another hormone-sensitive cancer. IVF involves progesterone to help the uterus get ready for an embryo, so could that increase risk? Most studies say no. A 2013 study of over 12,000 women found no rise in endometrial cancer after fertility drugs. Even a 30-year follow-up study showed that while infertility might bump up the risk, IVF itself doesn’t seem to add to it.
One exception? Women who use clomiphene citrate (a fertility drug sometimes used before IVF) for over six cycles might see a higher risk. But this is rare in modern IVF, where doctors usually switch to other meds if clomiphene doesn’t work.
Why the Confusion? Untangling the Myths
If the science is so reassuring, why do people still worry? Part of it is the mixed messages from early studies. Back in the 1990s, smaller studies hinted at a link between fertility drugs and cancer, but they didn’t account for things like infertility or lifestyle factors. Today’s bigger, better studies have cleared up a lot of that fog.
Another reason is fear of the unknown. Hormones sound intense—especially when you’re taking shots to rev up your ovaries. It’s easy to imagine they might mess with your body long-term. But here’s a fun analogy: Think of IVF hormones like a short, intense workout for your ovaries. It’s a big push, but then they rest. Cancer, on the other hand, is more like a slow burn that builds over years—not a quick sprint.
Interactive Quiz: Test Your IVF-Cancer Knowledge!
Let’s make this fun. Answer these quick questions to see what you’ve picked up so far:
- Does IVF increase your breast cancer risk, according to most studies?
A) Yes
B) No
C) Only if you’re over 40 - What’s more likely to raise ovarian cancer risk—IVF or never having kids?
A) IVF
B) Never having kids
C) Both equally - Can breastfeeding after IVF lower your cancer risk?
A) Yes
B) No
C) Only for ovarian cancer
(Answers at the end—don’t peek yet!)
Digging Deeper: 3 Things You Haven’t Heard About
Most articles stop at the big studies, but there’s more to this story. Here are three angles that don’t get enough attention—and they could change how you think about IVF and cancer.
1. The Timing Factor: When You Start IVF Matters
A lot of research lumps all IVF patients together, but what if your age when you start makes a difference? A study from Western Australia found that women who began IVF before 24 had a slightly higher breast cancer risk later on—possibly because their bodies were exposed to extra hormones during a key developmental window. Meanwhile, women over 40 didn’t show this pattern. It’s not a dealbreaker, but it suggests your life stage could tweak the risk in ways we’re just starting to understand.
Practical Tip: If you’re younger and considering IVF, talk to your doctor about spacing out cycles or monitoring your hormone levels closely. It’s not about avoiding IVF—it’s about tailoring it to you.
2. Your Infertility Type Might Play a Role
Not all infertility is the same. Endometriosis, polycystic ovary syndrome (PCOS), or unexplained infertility could each affect your cancer risk differently. For example, a 2018 UK study found that women with endometriosis who did IVF had a slightly higher chance of ovarian tumors. Why? Endometriosis itself is a risk factor—IVF might just amplify what’s already there.
Real-Life Example: Meet Sarah, a 35-year-old with PCOS who went through three IVF cycles. She worried about cancer because her condition already messes with her hormones. Her doctor explained that PCOS raises endometrial cancer risk a bit, but IVF doesn’t seem to pile on extra danger. Knowing her specific risks helped Sarah feel more in control.
Practical Tip: Ask your fertility specialist how your diagnosis might interact with IVF. A personalized plan beats a one-size-fits-all approach any day.
3. Long-Term Follow-Up Is Still a Work in Progress
Here’s something wild: Most IVF studies only track women for 10-20 years. But cancers like ovarian or endometrial often show up after age 60. The average IVF patient in those studies is in her 30s or 40s, so we’re missing data on what happens decades later. A Belgian study pointed out that ovarian cancer peaks at 66.5 years—way beyond most study timelines.
What does this mean? We can’t say IVF never affects cancer risk later in life—we just don’t have the full picture yet. It’s like watching a movie but leaving before the ending.
Practical Tip: If you’ve had IVF, keep up with regular cancer screenings as you age—pap smears, mammograms, the works. It’s a smart move no matter what.
Kids Conceived Through IVF: Are They at Risk?
Okay, so what about the babies? Some parents-to-be worry that IVF might affect their child’s health down the line. A 2010 study in Pediatrics found a 42% higher cancer risk in IVF kids compared to naturally conceived ones—but hold up. The actual risk was tiny (one extra case per 1,000 kids), and it included rare cancers like leukemia. Plus, the study couldn’t prove IVF was the cause—preterm birth and low birth weight (common in IVF) might be the real culprits.
More recent research, like a 2019 Dutch study of 24,000 IVF kids, found no increased cancer risk at all. The takeaway? Your little one’s probably just as safe as any other kid.
Parent Tip: Focus on a healthy pregnancy—good nutrition, rest, and prenatal care. That’s what matters most, IVF or not.
Hormones vs. Lifestyle: What’s Really Driving Risk?
Here’s a fresh angle: Maybe it’s not the IVF hormones we should worry about—it’s everything else. Infertility often comes with stress, weight gain, or delayed childbearing, all of which can nudge cancer risk up. A woman doing IVF might skip exercise during treatment or feel overwhelmed—habits that stick around longer than the hormone shots.
Simple Math: Let’s say infertility doubles your ovarian cancer risk (from 1% to 2% lifetime chance). IVF might not change that number—but gaining 20 pounds or smoking could push it to 2.5%. Lifestyle tweaks could outweigh the IVF effect entirely.
Action Step: During IVF, lean on stress-busters like yoga or walks with a friend. It’s good for your body and your mind.
Poll Time: What Worries You Most?
We’re curious—what’s on your mind when you think about IVF and cancer? Vote below and see what others say:
- A) Breast cancer risk
- B) Ovarian cancer risk
- C) My future kid’s health
- D) I’m not worried—bring on the facts!
(Share your pick in your head—or with a friend if you’re chatting about this!)
Busting Myths with a Checklist
Let’s clear up some common worries with a quick checklist. Here’s what’s true—and what’s not:
✔️ True: Infertility itself might raise cancer risk slightly, especially if you never have kids.
❌ False: IVF hormones automatically give you cancer—they’re short-term, not a lifetime dose.
✔️ True: Breastfeeding after IVF could lower your breast cancer risk.
❌ False: IVF kids are doomed to get cancer—the risk is tiny and unclear.
✔️ True: Regular checkups matter more as you age, IVF or not.
Your Game Plan: Steps to Feel Confident
So, you’re thinking about IVF—or maybe you’ve already done it. How do you move forward without the cancer question nagging at you? Here’s a step-by-step guide:
- Talk to Your Doctor: Ask about your personal risk factors—age, infertility type, family history. Get the real scoop, not just Google guesses.
- Know Your Hormones: Ask how many cycles you might need and what meds you’ll take. Fewer cycles mean less hormone exposure.
- Stay Healthy: Eat well, move your body, and manage stress. It’s not just about IVF—it’s about your whole life.
- Screen Smart: After IVF, stick to cancer screenings like mammograms or pelvic exams. Early detection is your superpower.
- Trust the Data: Remind yourself that decades of research lean toward “no big risk.” You’re not rolling the dice here.
Bonus Tip: Jot down questions before your next appointment—like “How does my PCOS affect this?” It’s your body, your call.
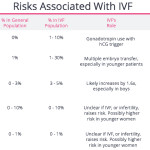
A Little Number Crunching: What’s Your Risk, Really?
Let’s put this in perspective with some quick, original math. Say the average woman has a 12% lifetime risk of breast cancer (1 in 8, per the American Cancer Society). Studies suggest IVF doesn’t bump that up significantly—maybe to 12.5% at most, if at all. For ovarian cancer, the baseline is 1.3%. Even with infertility, it might hit 2%—and IVF doesn’t seem to push it higher.
Compare that to lifestyle risks: Obesity can double your endometrial cancer odds, and smoking hikes lung cancer risk by 20 times. IVF’s tiny “maybe” pales next to those giants.
Real Stories: Voices from the IVF Journey
Meet Jen, a 38-year-old mom who did IVF five years ago. “I was terrified about cancer at first,” she says. “My aunt had breast cancer, so it felt personal. But my doctor walked me through the studies, and I focused on staying active during treatment. Now I’ve got a toddler and no regrets.”
Then there’s Mark, whose wife did IVF at 42. “We worried about her health, not just the baby’s. But she’s fine—still gets mammograms every year. It’s about balance, not panic.”
These stories show it’s not just numbers—it’s people living their lives, weighing risks, and finding peace.
The Future: What’s Next for IVF and Cancer Research?
Science isn’t done yet. Researchers are now looking at super-long-term effects—like what happens 40 years after IVF. They’re also studying newer techniques, like egg freezing or minimal-stimulation IVF, which use fewer hormones. Could these lower any tiny risks even more? Maybe.
There’s also buzz about genetics. Could your DNA—like BRCA mutations—interact with IVF in unique ways? It’s a frontier we’re just starting to explore.
Stay Tuned Tip: Follow health news or ask your doctor about updates. Knowledge is power!
Final Interactive: Your IVF Confidence Meter
Rate yourself—how confident do you feel about IVF and cancer risk now?
- 1: Still super worried
- 3: Meh, I get it but I’m cautious
- 5: Totally chill—bring on the baby!
(Reflect on your number—what’s holding you back or boosting you up?)
Wrapping It Up: Your Takeaway
IVF is a big decision, and wondering about cancer is totally normal. The science says it’s not a major risk booster— infertility itself might matter more than the treatment. Age, your health, and even when you start IVF could tweak the odds, but the overall vibe? Pretty safe. Arm yourself with facts, lean on your doctor, and live your life—not your fears.
Oh, and those quiz answers? 1) B, 2) B, 3) A. How’d you do?
You’ve got this—whether it’s IVF or just curiosity, you’re in the driver’s seat now. What’s your next step?