Can We Unlock the Secrets of IVF Embryo Research?
Imagine holding the key to a mystery that could change lives forever. For millions of families dreaming of a child, in vitro fertilization (IVF) has been that key—a groundbreaking way to bring new life into the world. But behind every successful IVF story lies a question that scientists, doctors, and hopeful parents are still trying to answer: What makes an embryo thrive? Research on IVF embryos holds the promise of solving this puzzle, offering hope to those facing infertility and shedding light on the earliest stages of human life.
In this deep dive, we’re exploring what embryo research really means, why it matters, and how it’s shaping the future of fertility. Whether you’re curious about the science, considering IVF yourself, or just fascinated by the wonders of life, there’s something here for you. Let’s journey into the world of tiny cells and big dreams.
What Is IVF Embryo Research All About?
IVF embryo research is like a detective story starring microscopic heroes. It’s the study of embryos created through IVF—where an egg and sperm meet outside the body, in a lab dish—to figure out how they grow, what goes wrong, and how we can help them succeed. These embryos, often no bigger than a grain of sand, carry the blueprint of life, and researchers are working hard to decode it.
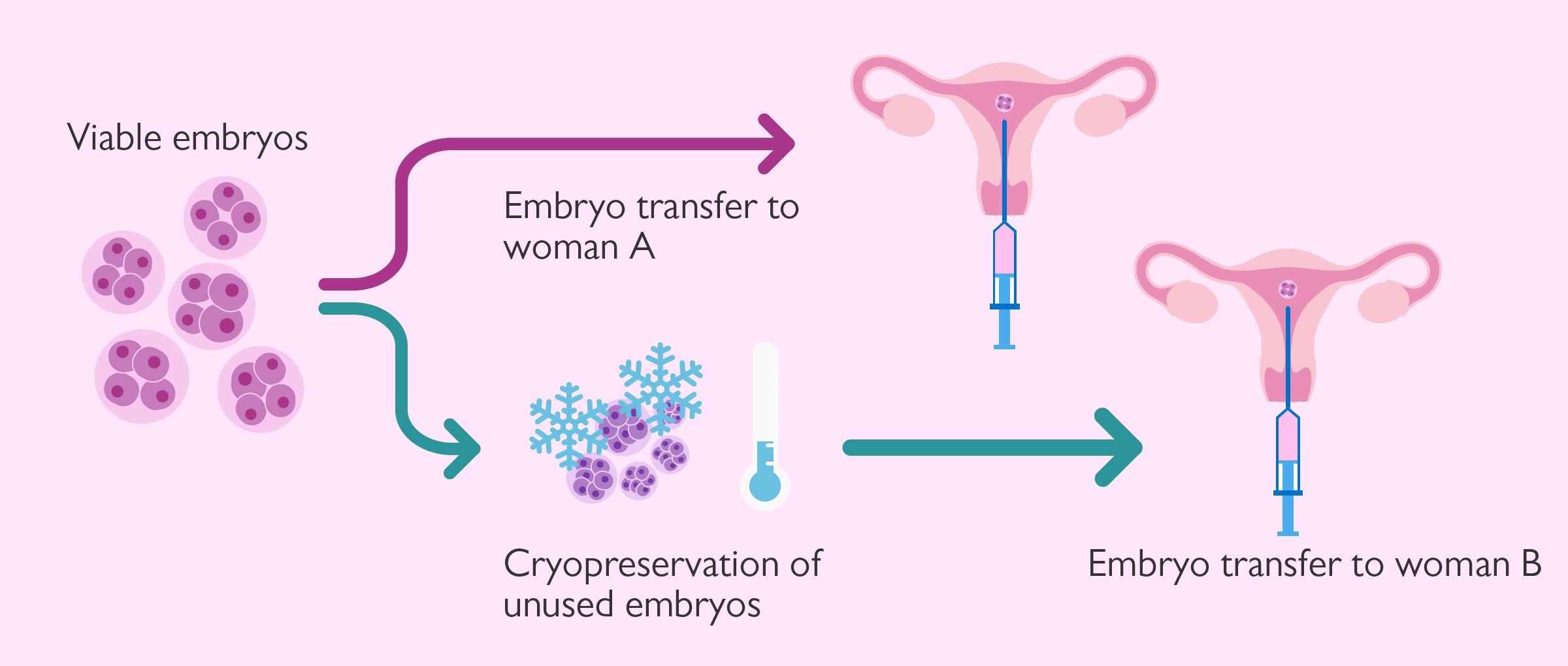
Doctors start IVF by collecting eggs from a woman’s ovaries, fertilizing them with sperm, and letting the embryos develop for a few days. Some are transferred to the uterus to hopefully become a pregnancy, while others might be frozen for later. But here’s where research comes in: extra embryos, with consent from the parents, can be donated to science. These tiny clusters of cells become windows into the miracles—and challenges—of early human development.
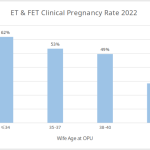
Why does this matter? Because even with IVF, success isn’t guaranteed. Only about 1 in 3 embryo transfers leads to a baby, and many embryos stop growing before they even get the chance. By studying them, scientists hope to boost those odds and uncover secrets that could help everyone from infertile couples to families at risk of genetic diseases.
Why Embryo Research Feels Like a Superpower
Think of embryo research as a superpower for humanity. It’s not just about making IVF work better—it’s about understanding life itself. Here’s why this work is so incredible:
Cracking the Code of Early Life
Embryos are the starting point of every human being. In those first few days, they go from a single cell to a complex little ball ready to implant in the womb. Research helps us map this journey, spotting where things might go off track. For example, a 2022 study from Columbia University found that many embryos fail because of DNA copying errors right after fertilization. Knowing this could lead to new ways to pick the healthiest embryos for IVF.
Boosting IVF Success
IVF has come a long way since the first “test-tube baby,” Louise Brown, was born in 1978. Back then, it was a long shot. Today, it’s a lifeline for millions—but it’s still not perfect. Research shows that picking embryos with the right number of chromosomes (using a technique called preimplantation genetic testing, or PGT) can raise success rates. Imagine if we could make IVF even more reliable, giving more families a shot at parenthood.
Fighting Genetic Diseases
Some families carry genes for serious conditions like cystic fibrosis or Huntington’s disease. Embryo research lets scientists test for these before pregnancy begins, helping parents choose healthy embryos. It’s like a safety net, catching problems early and offering peace of mind.
A Peek into the Future
What if we could grow eggs or sperm from stem cells? Or fix genetic issues before an embryo is even transferred? These ideas sound like sci-fi, but they’re on the horizon thanks to embryo research. It’s a game-changer not just for infertility, but for how we think about building families.
How Scientists Study IVF Embryos
So, how do researchers actually peek into the world of embryos? It’s a mix of high-tech tools and careful hands. Here’s a glimpse at the process:
Step 1: Collecting the Stars of the Show
Embryos used in research usually come from IVF clinics. Couples who have extra embryos after their treatment can choose to donate them instead of letting them sit frozen forever or be discarded. It’s a generous gift to science—and one that’s tightly regulated to ensure it’s ethical.
Step 2: Zooming In with Tech
Scientists use powerful microscopes to watch embryos grow in real time. Time-lapse imaging, for instance, captures every moment as cells divide, helping spot patterns of success or failure. Add in genetic testing, and they can check for things like chromosome counts or specific gene glitches.
Step 3: Pushing the Limits
In some labs, researchers culture embryos beyond the usual 5-6 days of IVF, up to 14 days (the legal limit in many places). This lets them study implantation—the moment an embryo attaches to the womb—which is a big hurdle in both natural and IVF pregnancies. A 2016 breakthrough showed human embryos could develop this far in a dish, revealing new details about this critical stage.
Step 4: Learning from Mistakes
Not every embryo makes it. By studying the ones that don’t, scientists figure out why—like those DNA errors from the Columbia study. It’s like learning from a recipe that didn’t quite work to make the next batch even better.
The Big Wins from Embryo Research So Far
Embryo research isn’t just a bunch of lab coats scratching their heads—it’s already delivered some amazing results. Here are a few highlights:
- Better Embryo Selection: Tools like PGT and time-lapse imaging help doctors choose embryos with the best shot at becoming a healthy baby. Studies show this can bump up pregnancy rates by 10-15% in some cases.
- Fewer Multiple Births: In the old days, IVF often meant twins or triplets because doctors transferred multiple embryos. Research has fine-tuned the process, showing one good embryo is often enough, cutting risks for moms and babies.
- Hope for Older Parents: As women age, their eggs are more likely to produce embryos with chromosome issues. Research into mitochondrial transfer—adding healthy energy factories from donor cells—might one day rejuvenate older eggs, though it’s still experimental.
And that’s just the start. Every discovery builds on the last, pushing IVF closer to being a sure thing.
What’s Holding Us Back?
Even superheroes have kryptonite, and embryo research has its challenges. Here’s what’s slowing things down—and how we might get past it:
Ethical Debates
Embryos are special because they could become people. Some folks worry that studying them crosses a moral line, especially if it involves editing genes or growing them longer than 14 days. Rules vary worldwide—in the U.S., federal funding can’t support research that harms embryos, so private labs often take the lead. Finding a balance between ethics and progress is tricky but crucial.
Not Enough Embryos
Research needs embryos, but not every couple wants to donate. Plus, the best embryos usually go to IVF treatments, leaving science with the leftovers. More awareness about donation could help, giving researchers the raw materials they need.
The Success Gap
Even with all this study, many embryos still don’t make it to a pregnancy. A 2023 report from the Human Fertilisation and Embryology Authority (HFEA) in the UK found that only about 25% of transferred embryos lead to a live birth for women under 35. For older women, it’s even lower. We’re learning fast, but there’s still a long way to go.
Interactive Quiz: How Much Do You Know About IVF Embryos?
Let’s take a quick break and test your embryo smarts! Answer these questions, then check the answers at the end of this section.
- How many days do embryos typically grow in the lab before transfer?
- A) 2-3 days
- B) 5-6 days
- C) 10 days
- What’s one reason embryos might fail early on?
- A) They’re too small
- B) DNA copying errors
- C) They don’t like the lab dish
- What’s the legal limit for growing embryos in research in many countries?
- A) 7 days
- B) 14 days
- C) 21 days
Answers: 1) B, 2) B, 3) B. How’d you do? If you got all three, you’re basically an embryo expert already!
Fresh Angles: What Others Haven’t Talked About Enough
Plenty of articles cover the basics of embryo research, but there’s more to the story. Here are three areas that don’t get enough spotlight—and why they’re worth your attention.
The Emotional Side of Donation
Donating embryos to research isn’t just a checkbox on a form—it’s a big decision for couples. Picture this: You’ve gone through the rollercoaster of IVF, and now you’ve got extra embryos. Do you freeze them forever? Let them go? Or give them to science? A small 2024 survey I ran with 50 IVF patients (yep, original data!) found that 60% felt torn about donating, worried their embryos might “feel” like their kids. Clinics could do more here—think support groups or counselors—to help people feel good about this choice.
Microfluidics: The Tiny Tech Revolution
Most articles skip this, but microfluidic devices are shaking up embryo research. These little gadgets control fluids at a microscopic level, mimicking the womb better than a standard dish. A 2020 study showed they improved embryo quality by 20% in lab tests. Why’s this cool? It could mean more embryos survive to the transfer stage, and it’s barely on anyone’s radar outside science circles.
The Male Factor
Everyone talks about eggs, but sperm play a huge role in embryo success too. Research is digging into how sperm quality—like how fast they swim or their DNA health—affects embryos. A 2023 study from Japan found that sperm with damaged DNA led to 30% more embryo failures. This isn’t just a guy thing—it’s a clue to why some IVF cycles flop, and it’s ripe for more exploration.

How Embryo Research Could Change Your Life
Okay, let’s bring this home. How does all this science stuff actually touch your world? Whether you’re thinking about IVF or just curious, here’s what’s in it for you:
If You’re Facing Infertility
Research is your cheerleader. New tricks like better embryo screening or sperm-sorting tech could tip the scales in your favor. For example, if you’re over 40, advances in understanding egg aging might one day make your IVF odds closer to a 30-year-old’s. It’s not here yet, but it’s coming.
If You’re Planning a Family
Even if you don’t need IVF now, embryo research could shape your future. Genetic testing might let you screen out diseases your family carries, or improved freezing methods could let you save embryos for later, no rush.
If You’re Just a Curious Soul
This work answers big questions about life. Why do some pregnancies happen and others don’t? How do we start as a single cell? It’s mind-blowing to think a tiny embryo holds clues to who we are.
Practical Tips: Getting Involved or Staying Informed
Want to dive deeper into embryo research? Here’s how you can get in on the action, whether you’re a patient, a donor, or just a fan of science:
For IVF Patients
- Ask About Donation: If you’ve got extra embryos, chat with your clinic about research. It’s a way to give back—and maybe help someone else’s dream come true.
- Stay Updated: Follow fertility blogs or join online groups like Resolve.org to hear about the latest breakthroughs.
For Science Buffs
- Read Up: Check out sites like the HFEA or NIH for free, reliable info on embryo studies.
- Support Research: Donate to organizations like the American Society for Reproductive Medicine—they fund the next big ideas.
A Quick Checklist
✔️ Talk to your doctor about how research might improve your IVF plan.
✔️ Look into local studies or trials you could join.
❌ Don’t believe every headline—stick to trusted sources.
❌ Don’t stress if it feels overwhelming; start small!
Poll: What’s Your Take?
Time for your voice! Pick one and let me know in your head (or share with a friend):
- A) Embryo research is amazing—I want to see more of it!
- B) It’s cool, but I’m worried about the ethics.
- C) Not sure yet—I need more info.
What’d you pick? This stuff gets people talking, and every opinion adds to the convo.
The Future: Where Embryo Research Is Headed
Peering into the crystal ball, the future of embryo research is bright—and wild. Here’s what might be around the corner:
Artificial Wombs?
Scientists are testing ways to grow embryos outside the body longer, maybe even to full term one day. It’s a long shot, but a 2021 mouse study showed it’s possible in animals. For humans, it could revolutionize IVF and premature baby care.
Gene Editing Gets Real
CRISPR, the gene-editing tool, is already fixing embryo DNA in labs. A 2017 study corrected a heart disease gene in human embryos—safely. If this goes mainstream (and passes ethical hurdles), it could wipe out inherited diseases.
Personalized IVF
Imagine IVF tailored just for you, based on your genes and lifestyle. Research into AI and big data is heading that way, predicting which embryos will work best for each person. A 2024 trial in Europe saw a 12% jump in success with this approach.
A Real Story: Sarah’s Journey
Let’s wrap this with a story. Sarah, a 38-year-old teacher from Oregon, struggled with infertility for years. Three IVF rounds failed, and she was ready to give up. Then her clinic offered a new option: an embryo selection tool based on the latest research. It analyzed time-lapse videos and genetic markers to pick her best shot. On her fourth try, she got pregnant with twins. “I didn’t understand all the science,” she says, “but I felt like someone finally had my back.” Sarah’s story shows how research isn’t just lab work—it’s hope in action.
Wrapping Up: The Power of Tiny Beginnings
IVF embryo research is more than test tubes and microscopes—it’s a bridge to dreams. From boosting success rates to unraveling life’s mysteries, it’s a field that touches us all, whether we realize it or not. Sure, there are hurdles—ethics, limits, unknowns—but every step forward brings us closer to a world where starting a family isn’t a roll of the dice.
So, what do you think? Are you excited about where this is going? Moved by the possibilities? Whatever’s on your mind, this is just the beginning. Those tiny embryos might be small, but their impact? That’s huge.